Managing Cardiovascular Emergencies in COVID-19 Pandemic: Challenges in Timely Diagnosis and Delivery of Care
Christoph W Sossou, Ariyon Schreiber, Neelesh Gupta, Chowdhury H. Ahsan
Division of Cardiology, Kirk Kerkorian School of Medicine and University Medical Center, Las Vegas, NV, USA
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARSCoV-2) infection leading to the novel coronavirus disease 2019 (COVID-19) has had an unprecedented impact on the cardiovascular system.
Among patients hospitalized with COVID-19, various cardiovascular manifestations such as myocardial injury, thrombosis, ACS, Type II Myocardial infarction, arrhythmia, shock and a wide range of cardiovascular complications have been documented (1-6). Various Testing abnormalities (e.g., ECG abnormalities, Transthoracic Echocardiography abnormalities, elevated cardiac biomarkers (cTn)) also have made the evaluation of COVID 19 patients increasingly difficult for clinicians.
The heterogeneous presentation of covid-19 patients coupled with the logistic issues of timely diagnosis and delivery of care, has made it challenging for clinicians more than ever before.
ACS and ACS-MIMICs in COVID-19 Patients
A vast number of patients who present to the hospital with COVID-19 have elevated cardiac biomarkers (cTn) indicating myocardial injury. Some of these individuals may also have ECG findings consistent with ST elevations and may not be necessarily truly ST elevation myocardial infarction (STEMI). Promptly, yet accurately discerning ACS (STEMI or NSTE-ACS) from STE-non-ACS (coronary vasospasm, acidosis, sepsis, electrolytes derangements, acute pulmonary embolism, etc.) is paramount as it gravely has therapeutic and prognostic implications.
Differentiating between type 1 (plaque rupture/erosions) and type 2 MI (myocardial supply demand mismatch due to a variety of reasons) is of great importance clinically as it can be problematic in this patient population with significant practical implications.
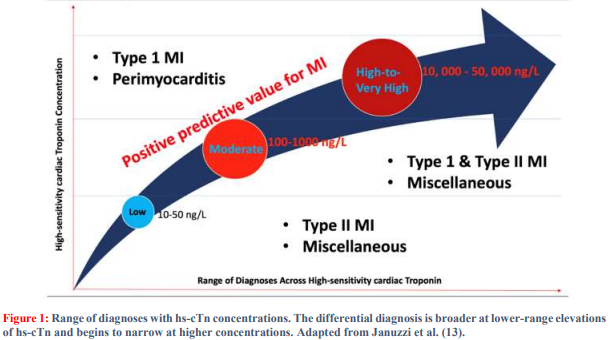
Astute clinicians must not only care for the patient before them, but ought to be great stewards of limited resources. Instead of using resources indiscriminately, with aid of symptoms, medical history, and judicious use of non-invasive diagnostic tests (ECG, cTn, TTE) at their disposal, clinicians must assess the probability of an individual patient having a plaque rupture and or plaque erosions. Though ST-elevation on ECG and positive cTn are indicative of acute myocardial injury, they do not within themselves reveal the underlying pathophysiologic mechanisms. Understanding the mechanism(s) of myocardial injury should guide the clinical decision-making, which impacts outcomes (See Figure 1).
Primary PCI is the standard of care for all COVID-19 patient presenting with ACS (STEMI or NSTE-ACS) regardless of their initial point of contact (non-PCI vs. PCI capable health center) (6-7). For patients with STEMI in whom rapid reperfussion with PPCI is not feasible (FMC-to-PPCI > 120 minutes), a pharmaco-invasive strategy followed by immediate transfer to PCI capable center for possible rescue PCI should be considered (8-9).
However, not all COVID-19 patients with STEMI will benefit from any reperfusion strategy or advanced therapeutic intervention (including the use of Mechanical Circulatory Support).
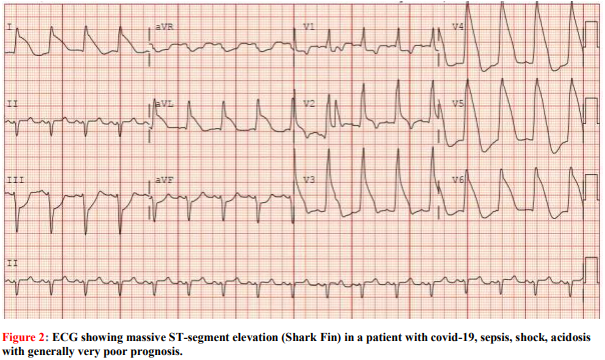
Figure 2 is an ECG of an individual who presented with severe COVID-19 and STEMI. Even though it can be tempting to revascularize every patient presenting with STEMI, individuals with confirmed COVID-19 who are felt to have an excessively high mortality (i.e., intubated in ICU, escalating vasopressors, worsening acidosis, multi-organ system failure, etc.), conversation regarding compassionate medical care between patient’s loved one and a multidisciplinary team should be initiated early. Frank, honest, and guarding patient’s loved ones’ expectations.
COVID-19 patients with equivocal diagnosis of ACS (STEMI or NSTE-ACS) due to atypical symptomatology, atypical ECG findings, or STsegment elevation not consistent with specific coronary territory, cTn without significant temporal changes (at least 50% change ? rise and/or fall from
.png)
compassionate conversation with patients loved one might lead to family-physician trust, fostering therapeutic alliance which might impact patient and/or family experience, improve resource stewardship, while maintaining clinical excellence. Treating patient is just as vital as baseline), further non-invasive evaluation is warranted. Current 5th generation cTn have high sensitivity for myocardial injury but lack specificity regarding mechanism of injury.
Hence, cTn below 10,000ng/L has a vast differential diagnosis but once cTn is equal or greater than 10,000 ng/L, the differential narrows down to acute myocardial infarction or myocarditis (See Figure 1) (13). Diagnostic and therapeutic decisions should be based on individual patient’s prognosis, guarded patients, and family wishes, as well as available resources and expertise at each health center.
COVID-19, STEMI and STEMI Mimics!
COVID-19, with its wide array of clinical presentations, can bewilder clinicians with STsegment elevation on ECG, which may not necessarily be due to acute ST-segment elevation MI.
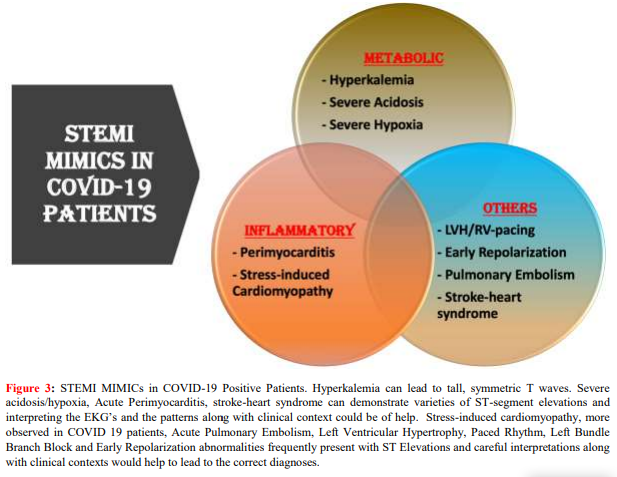
There are many conditions in covid-19 that can mimic STEMI such as acute perimyocarditis; severe hypoxia, acidosis and hyperkalemia; stress induced cardiomyopathy with apical ballooning; acute pulmonary embolism; early repolarization abnormalities raising concern for MI; and, rarely, COVID-19 related stroke manifesting as stroke heart syndrome with concomitant troponin elevation (Figure 3)
COVID-19 and Cardiogenic Shock
Patients with COVID-19 who developed cardiogenic shock are at higher risk of mortality during that index hospitalization (10-12). These subsets of COVID-19 patients tend to be older with multiple co-morbidities that portend worse outcome. Decision for early invasive strategy along with potential utilization of mechanical circulatory support (MCS) must be individualized based on patient’s characteristics, availability of resources and local expertise and assessment of overall prognosis by a multidisciplinary team.
Safety is Paramount
Cardiac catheterization laboratory personnel wellbeing is vital to excellent patient care. Safety of medical personnel should be Cath lab directors’ utmost concern. COVID-19 patients with cardiogenic shock requiring intubation are at the highest risk for droplet-based spread of COVID-19. Hence, every patient presenting during the COVID-19 pandemic with ACS (STEMI or NSTE-ACS) who requires an immediate invasive strategy should be deemed COVID-19 positive since reliable medical history is unattainable in these situations; not all regions have access to rapid diagnostic COVID-19 test.
Accordingly, appropriate masking of these patients and the use of personal protection equipment (PPE) and special precautions for high droplet components by all personnel is a must. It appears COVID-19 is here to stay; clinicians must learn to live with it. Protecting our patients and community starts with protecting our staff. Also, patients with covid-19 and cardiovascular disease should be evaluated by a multidisciplinary physician group to ensure that exorbitant resources are not utilized inappropriately on patients who may be better served by addressing the futility of care because of the presence of significant other comorbidities
1. Sandoval Y, Januzzi JL Jr, Jaffe AS. Cardiac troponin for assessment of myocardial injury in COVID-19: JACC review topic of the week. J Am Coll Cardiol. 2020; 76: 1244–1258
2. Kochi AN, Tagliari AP, Forleo GB, et al. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol. 2020; 31:1003–1008.
3. McCullough SA, Goyal P, Krishnan U, et al. Electrocardiographic findings in coronavirus disease19: insights on mortality and underlying myocardial processes. J Card Fail. 2020; 26:626– 632.
4. Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020; 5:802– 810.
5. 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults.
6. Chowdhury A, Christoph WS, and Jagat N. COVID-19 Cardiovascular Manifestations: Diagnostic Challenges and Therapeutic Ambiguities. J Inv Clin Cardio 2021; 3(2): 44-48
7. O 'Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guide- line for the management of STelevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Car- diol. 2013; 61:e78-e140
8. Larson DM, Duval S, Sharkey SW, et al. Safety and efficacy of a pharmaco-invasive reperfusion strategy in rural ST-elevation myocardial infarction patients with expected delays due to long-distance transfers. Eur Heart J. 2012; 33:1232-1240.
9. Dauerman HL, Sobel BE. Synergistic treatment of ST-segment elevation myocardial infarction with pharmacoinvasive recanalization. J Am Coll Cardiol. 2003; 42:646-651.
10. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 pa tients from Wuhan, China. Intensive Care Med. 2020; 46:846-848
11. Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323 (11):1061-1069
12. Alexis KO, Christoph SW, Neha SD., et al. “Coronavirus Disease 19 in Minority Populations of Newark, New Jersey - International Journal for Equity in Health.” BioMed Central, BioMed Central, 10 June 2020.
13. Januzzi JL Jr., Mahler SA, Christenson RH, et al. Recommendations for institutions transitioning to high-sensitivity troponin testing: JACC Scientific Expert Panel. J Am Coll Cardiol 2019; 73:1059–77.