Sickle Cell Treatment: A Multidisciplinary and Collaborative Clinical Redesign
Sadia K. Gazi,John Palumbo,Astou Seye,Monique Misra,Kristan Sikorski,Sheran M. Simo,Janis E. Bozzo,Kristin Edwards,Sheikh M. Hoq,Ryan T. O Connell
1Hospitalist Department, Bridgeport Hospital-Yale New Haven Health.
2 Department of Palliative Care, Bridgeport Hospital-Yale New Haven Health
3Department of Value Innovation and Shared Value Partnerships, Yale-New Haven Health
4 Department of Performance and Risk Management, Yale-New Haven Health.
Corresponding Authors: Sadia K. Gazi
Correspondence: Email: sadiagazi@gmail.com, 267 Grant St., Bridgeport, CT 06610.Background: Acute pain crisis is the most common reason for individuals with Sickle Cell Disease (SCD) to seek medical attention. The lack of a standardized treatment approach during pain crises leads to inefficient and costly care, resulting in a significant burden on the healthcare system.
Objective: To decrease inpatient length of stay and overall cost by redesigning the care of the SCD patient population.
Design: A retrospective original investigation involving a clinical redesign with multidisciplinary collaboration.
Setting: Bridgeport Hospital (BH), Bridgeport, CT, a member of the Yale New Haven Health System affiliated with Yale University School of Medicine.
Participants: All patients admitted to BH with pain crisis.
Interventions: Starting June 2015, patients at BH received treatment one of two ways: either in the ED per their pre-prepared treatment plan and were discharged to home, or were admitted to a specifically designated sickle cell service run by hospitalists in cooperation with a multidisciplinary team (where they initially received treatment with self-administered patient-controlledanalgesia) and were then transitioned back to their home oral regimen within a designated time period. Upon discharge, all patients were referred to follow-up at the newly established sickle cell medical home.
Main Measures: Length of stay and cost.
Key Results: Since the inception of the SCD program, average length of stay decreased by 36% (maximum of 68%), average cost per encounter decreased by 28% (maximum 61%), and average cost per patient decreased by 34% (maximum 73%). This has already garnered a savings of nearly $1,000,000. There was also a rise in the number of patients as the program attracted more SCD patients from the community to BH. Despite this increase, total ED visits decreased as did the number of overall admissions; concurrently, outpatient visits increased.
Conclusion: By redesigning the approach of treatment to the SCD population, hospitals can improve value in care.
Keyword: Sickle Cell Disease Acute pain crisis Opiate dependence Cost-effectiveness analysis Clinical Redesign Quality improvement.
Sickle Cell Treatment: A Multidisciplinary and Collaborative Clinical Redesign
Sadia K. Gazi,John Palumbo,Astou Seye,Monique Misra,Kristan Sikorski,Sheran M. Simo,Janis E. Bozzo,Kristin Edwards,Sheikh M. Hoq,Ryan T. O Connell
1Hospitalist Department, Bridgeport Hospital-Yale New Haven Health.
2 Department of Palliative Care, Bridgeport Hospital-Yale New Haven Health
3Department of Value Innovation and Shared Value Partnerships, Yale-New Haven Health
4 Department of Performance and Risk Management, Yale-New Haven Health.
Corresponding Authors: Sadia K. Gazi
Correspondence: Email: sadiagazi@gmail.com, 267 Grant St., Bridgeport, CT 06610.
Introduction
Sickle cell disease (SCD) is the most commonly inherited hemoglobinopathy characterized by the presence of sickle or crescent-shaped cells in the blood stream which result in hemolysis, vaso-occlusive phenomenon and a variety of serious organ system complications. Long term consequences that affect individuals with SCD include lifelong disability and premature death. Approximately 100,000 people are affected with this disease in the United States, the majority of which are African Americans1-2. SCD patients routinely experience life-threatening complications; therefore, they frequently visit the Emergency Department (ED) and often require admission to the hospital2 .
Research suggests that the SCD population is underserved and undertreated, with many studies demonstrating that the health system incurs millions in expenses from the repeated ED visits and hospitalizations, not to mention the cost to the patient’s own work productivity and overall financial condition3 . In 2004, more than 113,000 hospitalizations for sickle cell related illnesses were reported nationally—75% of which occurred in adults—totaling a cost of about $488 million. Out of that $488 million, 66% of the cost being carried by Medicaid and 13% by Medicare, indicating that the majority of cost burden falls upon the public healthcare fund1, 4 .
Patients with SCD typically lack access to appropriate outpatient care, as evidenced in an analysis of Medicaid data that showed this population to have utilized the ED as their safety net5 . Patients with the most ED visits also had the most inpatient hospital days and as a result had the greatest impact on healthcare costs5 . Similarly, another study demonstrated that hospitalizations of SCD patients originating from the ED had 20% higher cost on average than those stemming from other venues2 .
These findings highlight the dire need for a dedicated primary care program with steadfast engagement from healthcare providers for every individual suffering from SCD5 . At the same time, it shows that care in the emergency and inpatient setting is far from being optimized to handle the complex needs of patients with SCD6 . Pain is the hallmark feature of SCD and the major symptom for patients throughout their lives7 . The majority of patients consequently develop chronic physiologic dependence on opioids8 . Acute painful episodes are the most common reason for individuals with SCD to seek medical attention9 . Regardless of where in the spectrum of pain they fall, painful episodes are subjective and it is difficult to find objective clinical data to support patient report of pain. For this reason, negative attitudes toward individuals with SCD—along with clinician discomfort in prescribing frequent and higher dose opioids—can lead to inadequate treatment of pain which, in turn, can lead to frequent admissions and increased length of stay7 . The trend in frequent admissions for pain control can lead some clinicians to conclude that patients with SCD have a substance abuse disorder and that their request for pain medicine simply stems from addictive behavior10. This vicious cycle of undertreated pain combined with biased treatment leads many patients with SCD to feel misunderstood and judged by the medical community invariably resulting in a suboptimal experience11 .
Unfortunately, failure to recognize the complex psychosocial dynamics of subjective pain, physiologic dependence, and unconscious bias often contributes to the under treatment of pain and worsens the cycle of frequent admissions and prolonged length of stay. In 2015, a national report from the Academic Family Physicians noted discomfort among physicians in treating patients with SCD and that discomfort was highest among those who infrequently cared for SCD patients12. This highlights yet again the need for appropriate and dedicated management by those who have experience in this field in both inpatient and outpatient settings.
Bridgeport Hospital (BH) is a 383-bed hospital, part of the Yale New Haven Health (YNHH) System. At BH, patients with SCD demonstrated similar trends as mentioned above. Historically, patients with SCD admitted to BH for a pain crisis were randomly assigned to a hospitalist, making it unlikely for them to be familiar with their pain management requirements.
The hospitalists also did not use any standardized technique to determine how much pain medication a particular patient with SCD required, nor was there a set way to choose a particular opioid agent or route of administration. Hospitalists medicated patients based on their individual comfort level with opioid administration. Lack of continuity of care with the same hospitalist on subsequent admissions also led to redundant workup. These practice variations contributed to inadequate pain management, prolonged length of stay, high rate of readmissions, and increased frequency of ED visits not to mention the cost to the health system. The lack of a dedicated medical home also led patients to seek care in the ED for pain that could easily have been managed outpatient.
The YNHH system also identified that the SCD population contributed to a large portion of inpatient days at BH. Recognizing all the above-mentioned points, BH set up a clinical redesign with hospitalist leadership to decrease length of stay and cost in the SCD population. The clinical redesign was a multidisciplinary team-based approach to care: starting from first contact in the ED, following throughout the hospital stay, and facilitating the transition to long term outpatient care. Using a shared decision-making approach, palliative care clinicians guided the development of individual treatment plans with a focus on the ED and inpatient care with the ultimate goal of rapid and appropriate pain management to enable an early and safe discharge.
Methods
The study data was collected by retrospective review of the medical records. All patients with SCD whether known to BH (either through prior admission or ED visit) or new to the system since the initiation of this redesign in June 2015 were incorporated into the clinical redesign. Hospitalists partnered with the palliative care team to create a customized treatment plan (Appendix Figure 1) tailored to each individual SCD patient after interviewing them. The treatment plan provided a recommendation to ED providers regarding the preferred choice of analgesic, administration route, and dosage for patients with SCD visiting the ED with pain crisis. Further instructions were available to the admitting Hospitalist provider if decision was made to admit. The treatment plan was located as an FYI in the patient’s electronic medical record and accessible to all team members caring for the patient.
Per the treatment plan, a patient could receive up to 3 doses of intravenous pain medicine every 30 minutes as needed in the ED, after which they would be assessed for discharge or admission. Admitted patients were directed to a particular medical unit trained to care for SCD patients. Given the high intensity of care most patients with SCD require, as well as the recognized psychosocial issues prevalent in this patient population, unit nurses received education on the disease process and empathy training. The nurseto-patient ratio was also enhanced to accommodate these needs such that a single nurse was not assigned to more than one patient with sickle cell pain crisis at a time. A patient-controlled-analgesia (PCA) was used for the deliverance of pain medication in the initial 48- 72 hours of admission to decrease burden on nurses and allow patients to have independent control of pain medication administration. The PCA order had specifications on loading dose, lockout interval, frequency and maximum dose allowed in a 24-hour period. After the first 48-72 hours, patients were transitioned back to their baseline analgesic medication regimen.
In the SCD unit, daily bedside rounds with a multidisciplinary team were performed. The team was led by the hospitalists and included a palliative APRN as well as a nurse manager. The social worker and care coordinator also participated on initial visits and more frequently if patients had greater psychosocial needs. During rounds, patients were updated on goals of treatment for the day. Once off the PCA, discharge could be anticipated the same day or within the next 24 hours. The involvement of the nurse manager, social worker and care coordinator were crucial in identifying discharge barriers and arranging timely discharge. Once a week, a representative from the pharmacy and pastoral Care also rounded with the team to identify any inconsistencies in dosing or potential drug interactions and provide spiritual support respectively. A crucial component of the redesign was to create an outpatient medical home for for patients with SCD. At the time of discharge, patients were provided with a follow-up appointment within a week and enough medication to last them until the visit. BH initiated ambulatory visits in July of 2016 and the Sickle Cell Medical Home was officially established in October of 2016.
Data analytics were performed on all SCD patients (aged 21 to 84 years) having a principal and/or secondary ICD code for SCD (excluding sickle cell trait). The patients included both those being cared for as an inpatient at BH as well as treat-and-release patients at BH ED, or follow-up patients at the BH outpatient clinic. The number of visits and rates were calculated and trended using administrative data where a visit or encounter was defined as when a patient received care at any of BH’s settings. Patient level financial data were obtained to analyze cost of care.
A Fiscal Year (FY) was a 12-month period defined as October of one year through September of the next. Trending and rates were calculated using formulas in Microsoft Excel and statistical analyses such as t-tests & ANOVA were performed using R-language (R Foundation for Statistical Computing). Results are typically reported as mean ± standard error of the mean (SEM) with * p < 0.05, ** p < 0.01 and *** p < 0.001.
Results
Demographics
For the time period of October 1, 2013 (Quarter 1, FY2014) through June 30, 2018 (Q3, FY2018) there were 521,025 hospital system encounters of which 1,368 involved patients with SCD. Of them, 155 were unique patients identified with an ICD code of interest (Table 1). Male-to-female ratio was about 1:2. An overwhelming majority (i.e. more than 90%) were African Americans. The average age of these patients was 35-36 years, with a median of 32-33 and a range from 21 to 84. Majority of the patients had Medicaid only insurance (53-57%) with the remaining mainly split between Medicare and Commercial insurance. All of these trends were similar before and after the inception of the SCD Program during Q3, FY2015. We therefore present pre-SCD program data from Q1 FY 2014 to Q3 FY2015 (i.e. 21 months) and post-SCD data from Q4 FY2015 to Q3 FY2018 (i.e. 36 months).
Trending of Utilization
We divided the encounters into three different settings: inpatient admissions, ED visits (treat-and-release) and outpatient visits. Since the implementation of the SCD program, we observed a decrease in the number of encounters/patient every month for both inpatient and ED settings (12% and 52% respectively) (Table 2). A concomitant 19% rise was noticed in the number of outpatient clinic visits/patient every month. The detailed trend per FY is shown in Figure 1.
We also noted a dramatic 36% reduction in the Average Length of Stay (ALOS) per admission since the beginning of the program from 9.8 days to 6.3 days (Table 2). However, a more drastic reduction is noted if comparing the peak ALOS in the pre-SCD program period (11.8 days) during Q2 FY2015 and the lowest point post-SCD program (3.8 days) in Q3 of FY2018 (Figure 2). This is a reduction of 8 days per admission or 68% (p < 0.01). Whereas the average trend line is noted to increase pre-SCD program implementation, this is clearly reversed following the initiation of the program (Figure 2)
Cost Analyses
We further noted a 26% reduction in the average direct cost per inpatient admission since the inception of the program (Table 2). There was similarly a 30% reduction in outpatient visit cost. However, we did observe a 12% increase in cost per ED visit.
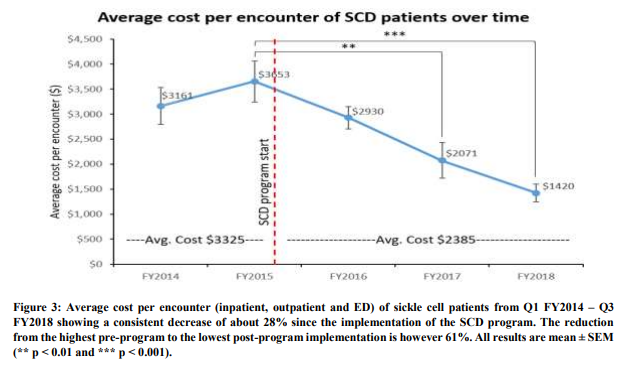
Overall, the number of encounters/patient every month decreased by about 17% while the average direct cost per encounter was curtailed by 28% ($3,325 to $2,385 – i.e. a reduction of $940 per encounter) (Table 2 and Figure 3). Therefore, given that we have had 1,020 encounters since the inception of the SCD program, this totals a savings of nearly $1,000,000 over 36 months. These numbers are however based on the average cost during the pre-SCD program period vs. post. If we instead looked at the average cost trend over time, we would see an ongoing steady decrease implying the savings would be even greater in the future (Figure 3 and Figure 4). In fact, the peak cost of $3,653 was noted just prior to the start of the SCD program whereas the lowest point of $1,420 was during our last data point in FY2018 (p < 0.001) (Figure 3). This is a reduction of $2,233 per encounter, which is a significant 61% in cost reduction when compared to the average cost reduction of 28% mentioned above. The average cost per patient was analyzed similarly and also demonstrates an average reduction by about 34% with a maximum of 73% from $18,335 prior to the program debut down to $4,947 at the end (p < 0.001) (Figure 4).
Table 1: SCD patient demographics from October 2013 (Q1 FY2014) to June 2018 (Q3 FY2018). Pre-redesign was from Q1 FY2014 to Q2 FY2015 (21 months) and post-redesign from Q3 FY2015 to Q3 FY2018 (36 months)
.png)
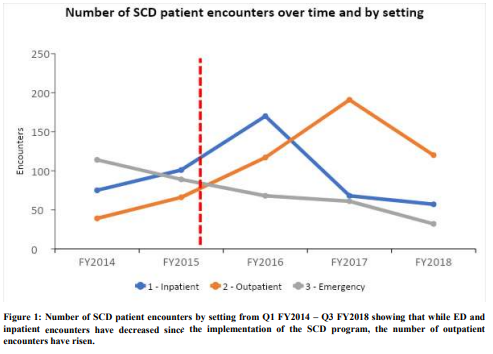
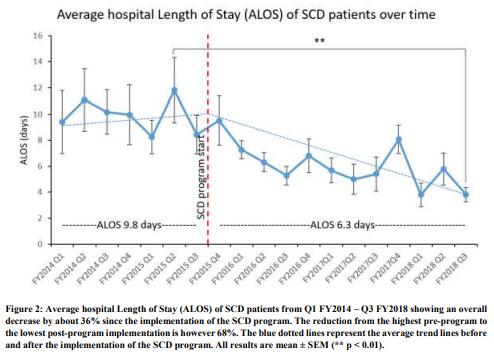
Table 2: Sickle Cell Disease patient utilization by setting from October 2013 (Q1 FY2014) to June 2018 (Q3 FY2018). Pre-redesign was from Q1 FY2014 to Q3 FY2015 (21 months) and post-redesign from Q4 FY2015 to Q3 FY2018 (36 months).
.png)
pt – patient, ALOS – Average Length of Stay. Raw numbers, in ( ), are totals observed over 21 and 36 months of Preand Post-SCD program periods respectively
.png)
Discussion
This clinical redesign acknowledged and addressed the multiple and complex challenges of caring for the SCD patient population. Firstly, it recognized this population as underserved and often misunderstood. Using a shared decision-making process, the creation of individualized treatment plans helped standardize treatment as well as form trusting relationships and therapeutic alliances with each patient. Second, the clinical redesign helped focus appropriate care at the right time and place for these patients. By standardizing the ED and inpatient care and creating more organized discharge plans, BH has been able to establish the much-needed shift of care in the SCD population from inpatient to outpatient.
With regards to inpatient admissions, the ALOS was significantly reduced by more than 36% with a maximum reduction of 68%. Similarly, the overall cost per encounter was also dramatically reduced by 28% with a maximum reduction of 61%. A maximum of 73% is seen when looking at the average cost reduction per patient. Over the course of the 36 months post-implementation of the SCD program, BH has thus saved nearly $1,000,000. Given the steady decrease in the cost over time, we could only expect a much higher rate of savings in the future.
Interestingly, while the average direct cost per inpatient admission as well as outpatient visit since the inception of the program has significantly decreased, we did observe a small 12% increase in the average cost per ED visit. However, the overall number of ED visits/patient every month has decreased by a significant 52%. Taken together, we believe that these fewer ED visits were of more serious nature and that the created treatment plans required more ED interventions in order to prevent unnecessary admissions
The initial rise seen in inpatient admissions after the onset of the SCD program during Q4 FY2015 (Figure 2) is explained primarily by the fact that the outpatient setup was not officially established until Q4 of FY2016-Q1 FY 2017 (i.e. an entire year after SCD program began). Once the outpatient setting was fully functional, the inpatient admissions drastically diminished as expected. By unifying the patient’s care under the umbrella of the hospitalist department, continuity of care was maintained even outside of the inpatient setting. The familiarity helped swiftly accelerate the discharge process; then, once the clinic was established, the process was made even easier. The ED was therefore no longer being used as a safety net—rather, it was used for true emergencies and severe symptoms
The clinical redesign team did indeed experience some apprehension and obstacles in creating this program. A major concern was that providing higher doses of opioids would lead to a more significant problem with dependency and addiction. The clinical expertise of the palliative care team was essential in providing education and creating an attitudinal shift towards opioid use in this patient population. Most patients who have pain crisis severe enough to warrant hospitalization use pain medication at baseline and therefore have physiologic tolerance. The prescribing clinicians received education that the inpatient opioid dosage should be at a minimum equi-analgesic to the patient’s baseline requirement, and increased in times of pain crisis. Throughout the redesign, we did not see any significant increase in pain medication requirements for our patients after the pain crisis was over, and the majority, if not all, were able to comfortably return to their baseline requirements once treatment was completed. All patients were counseled that they may never be completely free of pain and that a minimum level of tolerable pain should be set and targeted on their pain scale, usually around a 5 out of 10. Expectations were set that the goal was to achieve pain relief sufficient for comfort during daily activities and a normal lifestyle, but not necessarily to be completely pain free. The continuity of care in the outpatient clinic allowed us to wean opioids whenever possible and desired. During the years of this clinical redesign, we witnessed our SCD patients celebrate many life events: these included school graduations, return to employment, and marriage proposals. With education, the discomfort surrounding opioid prescription by hospitalists virtually disappeared. With the establishment of the clinic, most patients did not even require new prescriptions upon discharge, but rather resumed outpatient prescriptions they had already filled.
Individuals with SCD are well known to be at risk of psychosocial issues. Nurses and physicians alike were counseled regarding how to manage difficult situations. We established behavior expectations for our patients including respect and attention to the medical team, participation during rounds by turning off the television, telephones, and handheld devices. Because the PCA was available, we did not allow patients to page the overnight covering team for increases in pain medication beyond what was built into the PCA orders. Nurses and physicians monitored for signs of overuse and sedation as well as potential opioid misuse behaviors. In an effort to decrease the euphoria that can accompany IV opioid bolus administration, all opioids were provided through PCA (smaller incremental administration) or oral routes. All patients who had no contraindications were transitioned to oral opioids past the initial 48-72-hour window. Most recently, we have moved towards administration of opioids via subcutaneous route as the preferred route. The standard use of opioids in this fashion discouraged those who might seek the hospital for opioid misuse. Clinician burnout was also prevented by rotating the hospitalists on the SCD service after the initial establishment phase. Finally, other specialists who provided care to patients with SCD were encouraged to transfer further inpatient care to the hospitalists to maintain consistency given the success of the program.
In all, by identifying patients with SCD as a population with unique needs, much can be done to add value to their care. At BH, we were able to decrease length of stay and cost by implementing a clinical redesign that standardized the approach to treating pain with a treatment plan created based on the patient’s specific needs during a pain crisis. The addition of a dedicated outpatient medical home also provided substantial support to prevent recurrent admissions and unnecessary usage of the ED.
Conflicts of Interest
The authors have no conflict of interest.
Acknowledgements
This clinical redesign was sponsored by Michael Ivy, MD, Chief Medical Officer of Bridgeport Hospital. We would like to thank John Skelly, Vice President of Finance, for his support. We would like to thank the sickle cell team William Sotire, RN, Christine Russell, RN MSN, and Ellen Massey, LCSW, without whose hard work and dedication this redesign would not be possible. Special thanks to Nursing Director Peggie Parniawski, MSN, Chief Nursing Officer Maryellen Kosturko, MAHSM BSN RN and Project Manager Lynda Cook, MSN RN-BC
1. Singh, R., Jordan, R., and Hanlon, C. 2014. Economic Impact of Sickle Cell Hospitalization. Blood, 124(21), 5971.
2. Mayer, M.L., Konrad, T.R., Packard, L.S., Dvorak, C.C. 2003. Hospital Resource Utilization among Patients with Sickle Cell Disease. Journal of Healthcare for the Poor and Underserved, 14(1), 122- 135. DOI: 10.1353/hpu.2010.0834
3. Taylor, L.E., Stotts, N.A., Humphreys, J., Treadwell, M.J., Miaskowski, C. 2010. A review of the literature on the multiple dimensions of chronic pain in adults with sickle cell disease. Journal of Pain and Symptom Management, 40(3), 416-435. DOI: 10.1016/j.jpainsymman.2009.12.027.
4. Steiner, C.A. and Miller, J.L. 2006. Statistical Brief #21: Sickle Cell Disease Patients in US Hospitals, 2004. Healthcare Cost and Utilization Project, www.hcup-us.ahrq.gov/reports/statbriefs/sb21.jsp.
5. Blinder, M., Duh, M., Sasane, M., Trahey, A., Paley, C., and Vekeman, F. 2015. Age-Related Emergency Department Reliance in Patient with Sickle Cell Disease. The Journal of Emergency Medicine, 49(4), 513-522.
6. Kauf, T., Coates, T., Huazhi, L., Mody-Patel, N., and Hartzema, A. 2009. The Cost of Health Care for Children and Adults with Sickle Cell Disease. American Journal of Hematology, 84(6), 323-327
7. Zempsky, W.T. 2010. Evaluation and Treatment of Sickle Cell Pain in the Emergency Department: Paths to a Better Future. Clinical Pediatrics: Emergency Medicine, 11(4), 265-273. DOI: 10.1016/j.cpem.2010.09.002
8. Ruta, N.S., Ballas, S.K. 2016. The Opioid Drug Epidemic and Sickle Cell Disease: Guilt by Association. Pain Medicine, 17, 1793-1798. DOI: 10.1093/pm/pnw07
9. McClish, D.K., Smith, W.R., Dahman, B.A., Levenson, J.L., Roberts, J.D., Penberthy, L.T., Aisiku, I.P., Roseff, S.D., and Bovbjerg, V.E. 2009. Pain Site Frequency and Location in Sickle Cell Disease: The PiSCES Project. Pain, 145(1-2), 246-251.
10. Brown, S-E., Weisberg, D.F., Balf-Soran, G., and Sledge, W.H. 2015. Sickle Cell Disease Patients With and Without Extremely High Hospital Use: Pain, Opioids and Coping. Journal of Pain and Symptom Management, 49(3), 539-547.
11. Lattimer, L., Haywood, C., Lanzkron, S., Ratanawongsa, N., Bediako, S.M., Beach, M.C. 2010. Problematic hospital experiences among adult patients with sickle cell disease. Journal of Healthcare for the Poor and Underserved, 21(4), 1114-1123. DOI: 10.1353/hpu.2010.0940.
12. Mainouse, A., Tanner, R., Harle, C., Baker, R., Shokar, N., and Hulihan, M. 2015. Attitudes toward Management of Sickle Cell Disease and Its Complications: A National Survey of Academic Family Physicians. Anemia, 2015, 1-6. DOI: 10.1155/2015/853835
.png)