Global Health in Bangladesh - Surgical Outreach for Congenital Cleft Deformity Repair
Abrar Shamim, Shahid R. Aziz
1Columbia University, New York, NY, USA
2 Department of Oral and Maxillofacial Surgery, Rutgers School of Dental Medicine, Newark, NJ, USA; Division of Plastic and Reconstructive Surgery, Department of Surgery, Rutgers - New Jersey Medical School, Newark, NJ, USA
Funding Support: None
Acknowledgements: : The authors would like to thank Anette Wu, MD, MPH, PhD (Columbia University, College of Physicians and Surgeons) and Maisha Shamim, MD (Stony Brook Children’s Hospital) for their helpful review of this manuscript.
Disclosure: The authors claim no disclosures or conflict of interest. The manuscript has been read and approved by all authors. Requirements for authorship have been met. The presented information is not provided in another form.
Ethical Approval: Not applicable
Corresponding Authors: Shahid R. Aziz
Correspondence: Shahid R. Aziz, DMD, MD, FACS, FRCS(Ed) is an oral and maxillofacial surgeon and founder of Smile Bangladesh, Email: azizsr@sdm.rutgers.edu, Abrar Shamim is a student at the Columbia University College of Dental Medicine and volunteer for Smile Bangladesh.
Introduction
Over 5 billion people lack access to safe and affordable surgical care, with much of the burden on low and lowermiddle-income countries (LMICs), particularly in regions of Africa and the South Asian subcontinent 1 . Before the Coronavirus-19 (COVID-19) pandemic, an estimated 250,000 operations were conducted globally by visiting international surgical teams per year, however the pandemic has caused significant interruptions to these efforts due to international travel restrictions and reallocation of resources toward managing the pandemic 2 . The National Institute for Health and Care Research (NIHR) Global Health Research Unit on Global Surgery reports that there is a global backlog of 28 million surgical cases due to the pandemic 3 . Discrepancies in global surgical care, especially specialty surgical services, including oral and maxillofacial surgery, disproportionately affect underprivileged populations in LMICs and these inequalities are expected to grow following COVID-19.
In Bangladesh, there are approximately 300,000 patients with unrepaired facial clefts, often from underprivileged families, and only a handful of qualified surgeons to treat them4 .
These deformities may be managed by surgeons with expertise in the head and neck region, including oral and maxillofacial surgeons, plastic surgeons, or ENTs, often with specialized training in cleft and craniofacial surgery. The timing of care for patients with congenital conditions such as facial clefts, club foot, and congenital heart disease is critical as there are significant benefits to early intervention 2 . The shortage of qualified and geographically accessible surgeons for these patients, especially those located in rural areas of Bangladesh, is a major barrier to seeking and obtaining timely treatment during childhood. Orofacial clefts are a group of highly restrictive deformities because children have difficulty achieving proper nutrition via nursing and may be ostracized due to their appearance, resulting in difficulties integrating into society. General population knowledge on this condition varies widely, with some affected families holding superstitious beliefs as to the causes of facial clefts while others being simply unaware of potential surgical repair5 .
Cleft Repair in Bangladesh
To address the clear discrepancy between the surgical needs and available services in Bangladesh, both domestic and international efforts have been enacted to combat this problem. Cleft Bangladesh6 , a cooperation between international NGOs (based in Germany and Australia) and Bangladeshi NGOs, aims to increase access to surgical cleft repair services via operations in local hospitals and missions throughout the country. Smile Train7 is another internationally known nonprofit organization founded in 1999 based in New York City, which has provided cleft surgeries for children in 87 countries worldwide, including Bangladesh. These operations are conducted at 2 hospitals, located in Dhaka and Chittagong. The UKbased charity organization CLEFT8 has conducted missions and outreach for cleft repair and is working to improve comprehensive cleft care at the Sheikh Hasina National Institute of Burns and Plastic Surgery based in Dhaka. There are some, albeit limited, government funded health services providing cleft care. Bangladeshi doctors have also enacted domestic surgical missions, however they acknowledged that without international support, even their best efforts are insufficient to address the massive inequalities in surgical access 9 .
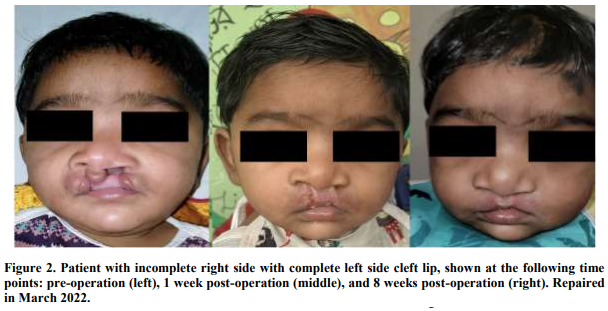
To address gaps in surgical care that have persisted in Bangladesh, we have founded Smile Bangladesh, a nonprofit organization founded with the purpose of addressing the incongruity between current needs and available services in cleft care in Bangladesh. Since 2006, over 25 missions have been led by the founder, facilitating the repair of 1600+ facial clefts and other craniofacial deformities. Our team is variably composed of volunteers including surgeons, anesthesiologists, nurses, and others, depending upon the sites to be visited, the local contacts and providers available for partnership, and the available resources (for example, the team will require independent anesthesiologists if the mission is taking place in rural Bangladesh, but may not if operating out of a Dhakabased facility). The COVID pandemic led to cancellation and postponement of many humanitarian aid missions, including those of Smile Bangladesh. Following four cancelled missions, Smile Bangladesh restarted its outreach missions in March 2022, during which a total of 37 surgeries (31 facial clefts and 6 orthognathic deformities) were performed. In this mission, 1 (2.7%) post-operative complication involving wound dehiscence was reported, which was
managed by the team’s local contacts, which demonstrates the importance of partnership with incountry providers. Perioperative outcomes are favorable, with non-life-threatening complications such as dehiscence or surgical site infections occurring in less than 5.5% of cases in written reports of previous missions4 and estimated to be similar in recent missions. The authors note that patients may be lost to follow up following the missions, impeding long-term data collection. In recent years, funding and resources for humanitarian missions have shifted toward a more sustainable model by supporting local healthcare frameworks and training local providers to encourage longitudinal improvement, especially in surgical care10 . Smile Bangladesh has adapted to this paradigm change by increasing its emphasis on educational efforts and increasing collaboration with local trainees and providers. In recent missions, operations have been live-streamed with audio and video to residents, surgeons, and professors in Bangladesh along with question-and-answer during the surgeries. Seminars and workshops have also been conducted by members of the team.
Developing a Cleft Repair Mission
The construction of a volunteer medical mission to an LMIC such as Bangladesh requires significant planning, which includes forming a clear mission statement, selecting a site location, determining funding sources, assembling a team, and establishing local contacts 11. It is important to have some members of the team who are familiar with cultural and social dynamics, who may also function as translators to ensure that the visiting team’s intentions may be clearly portrayed without risking offending local hosts or communities. For example, if a specialized surgical team arrives on a mission to repair facial clefts but fails to acknowledge or address other unmet local needs affecting a greater number of people, locals may wonder why a small cohort of patients with congenital deformities are receiving so much attention. Cognizance of such perceptions and cultural sensitivity are therefore needed to efficiently reach the mission’s goals.
Additionally, the closure of local facilities or postponement of scheduled procedures to host the visiting surgical team may lead to loss of income for local providers and importantly, delayed treatment for their patients. These considerations must be taken into account when scheduling and coordinating fly-in outreach missions with local hosts.
Securing funding from various sources is critical, especially for surgical missions, due to the cost of supplies and dispensables that are required to provide safe and standard-of-care treatment. Necessary supplies include specific instruments required to perform cleft repair and oral and maxillofacial surgery, medications for pain management, anesthesia, and infection control, disinfectant solutions and equipment, basic surgical supplies including gauze, sutures, etc., and supplies to treat potential complications including head/neck infections or wound dehiscence. It is estimated that the cost of performing one cleft repair surgery in Bangladesh is $350 and the overall cost of each mission is $40,000
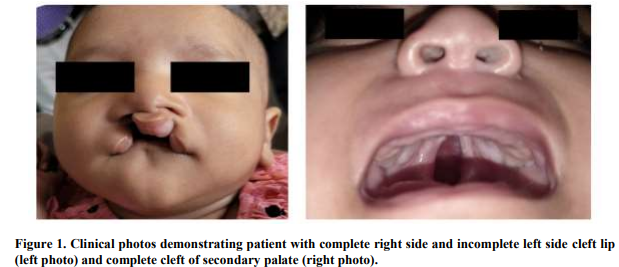
In classical medical missions to LMICs, these costs are often assumed by the team and its funders, however the team should remain aware of any costs or losses being inadvertently directed to local providers, which may be avoided with proper coordination between the team manager and local partners. The duration and types of surgical procedures for each repair vary based on whether the lip deformity is unilateral or bilateral, complete (entire vertical height of lip extending into the nasal cavity) or incomplete (confined to the lip), and whether there is additional involvement of the primary and/or secondary palate, which may extend posteriorly to the uvula (some deformities shown in Figure 1).
It is imperative to prioritize patient safety, organization, and postoperative care, longitudinally if possible. The basic tenets of medical ethics, including nonmaleficence and beneficence, must be maintained and the visiting team must provide standard-of-care treatment while upholding principles of ethics and code of conduct. Recent literary work has emphasized the need for host country collaboration and adequate record keeping by short term medical missions 12 . A universal electronic medical record system is still in its infancy in Bangladesh, with the country now working towards adding National ID (NID)/birth registration number into its healthcare systems, which provides a method for longitudinal follow-up and outcomes analysis. Additionally, interaction with the visiting medical team may be the only point of patient’s healthcare utilization, so integration with a medical record may be an opportunity to direct patients to other providers if necessary. For example, a patient with facial deformity presenting during screening may be referred for genetic testing if syndromic etiology is suspected. The authors note that adaptation to developing Bangladeshi infrastructures will facilitate future online and offline correspondence and long-term follow up, supporting the overall growth of the missions, but more importantly, supporting the developing systems of an emergent nation. As Smile Bangladesh has been conducting missions for many years and is known throughout the country, patients often revisit the international team who had treated them, sometimes several years back, however many patients are also lost to follow up. The next mission, scheduled for November 2022, is expected to encompass such follow-ups and surgeries previously postponed to accommodate recommendations for well-timed intervention, among other cases.
Conclusion
There was a time when specialty services such as infectious disease and obstetrics were the extent of Global Health1 . It has become clear that surgical services are an undeniable part of Global Health, which entails the health of all people, especially those in LICs and LMICs. In its infancy, global surgery was recognized solely as mission trips to countries with unmet needs10 . As the field evolves, global surgery will require innovation and cooperation to continue delivering surgical care in low-access areas while simultaneously supporting the development of long-lasting surgical health systems in LMICs such as Bangladesh10. The COVID-19 pandemic provides a challenge that may facilitate rapid technological change, further allowing these challenges to be faced head on. We encourage readers and educators to consider how remote services may be used to provide sustainable methods of teaching and surgical simulation or augmented reality, thereby allowing providers from LMICs to learn without traveling, and allowing willing educators from HICs to combat the phenomenon of “brain drain” (migration of physicians from low-resource to high-resource settings) without relocating13. We also encourage the readers of this journal to participate and contribute to surgical outreach missions, which should be enacted with an emphasis on ethical healthcare delivery in a manner that promotes independent growth and prosperity, not dependence or complacence.
With the context from this perspective article, the authors look forward to the participation of readers by means of financial support or interpersonal outreach that will help support future missions (by Smile Bangladesh or others) and address inequalities to healthcare access in Bangladesh.
1. Meara, J. G. et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet 386, 569–624 (2015).
2. Villavisanis, D. F., Kiani, S. N., Taub, P. J. & Marin, M. L. Impact of COVID-19 on Global Surgery: Challenges and Opportunities. Annals of Surgery Open 2, e046 (2021).
3. COVIDSurg Collaborative. Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. British Journal of Surgery 107, 1440–1449 (2020).
4. Aziz, S. R., Rhee, S. T. & Redai, I. Cleft Surgery in Rural Bangladesh: Reflections and Experiences. Journal of Oral and Maxillofacial Surgery 67, 1581– 1588 (2009).
5. Wessel, J. H., Ziccardi, V. B., Aziz, S. & Chuang, S. K. The Cleft Deformity in Bangladesh: A Descriptive Summary. Journal of Oral and Maxillofacial Surgery 71, e44 (2013).
6. Cleft Bangladesh: Cleft Bangladesh. https://www.cleftbangladesh.org/.
7. The World’s Largest Cleft Charity | Smile Train. https://www.smiletrain.org/.
8. Bangladesh. Cleft https://www.cleft.org.uk/pages/category/bangladesh.
9. Ghani, S., Mannan, A., Sen, S. L., Uzzaman, M. & Harrison, M. The problems of establishing modern cleft lip and palate services in Bangladesh. The Journal of Surgery 2, 43–47 (2004).
10. Nagengast, E. S. et al. The Local Mission: Improving Access to Surgical Care in Middle-Income Countries. World J Surg 45, 962–969 (2021).
11. Padmanaban, V., Hoffman, D., Aziz, S. R. & Sifri, Z. C. Developing a Sustainable Program for Volunteer Surgical Care in Low-Income and Middle-Income Countries. Oral Maxillofac Surg Clin North Am 32, 471–480 (2020).
12. Tracey, P. et al. Guidelines for short-term medical missions: perspectives from host countries. Globalization and Health 18, 19 (2022).
13. Dohlman, L., DiMeglio, M., Hajj, J. & Laudanski, K. Global Brain Drain: How Can the Maslow Theory of Motivation Improve Our Understanding of Physician Migration? Int J Environ Res Public Health 16, E1182 (2019).