Pilot Evaluation of AAFP TIPSTM continuous glucose monitoring (CGM) learning module for CGM Implementation into Primary Care
Mosleh Ahmed,Nancy Rodriguez,Ayesha Khan,Ammy Ghosh
Corresponding Authors: Mosleh Ahmed
Correspondence: PGY-3, Family Medicine, Jackson Park Hospital, Chicago, Email: muahmedshakil@gmail.com
Introduction
- With 28.7 million people of all ages or 8.7% of the US population diagnosed as diabetic, monitoring blood sugars is of paramount importance.
- Cumbersome needle pricks for glucose measurement paved the way of first continuous glucose monitoring (CGM) system approval by FDA in 1999.
- Today’s CGM systems are small wearable devices that track glucose around the clock, typically checking levels every few minutes.
- Generally, CGM devices contain 3 components: sensor, transmitter & receiver. Sensor contains a minute wire inserted just under the skin on the stomach, back of the arm or leg.
- Sensor communicates wirelessly with a receiver or smartphone app display via a transmitter.
- The system allows the patient and caregivers to monitor glucose patterns in real time.
- Depending on loop connection with insulin delivery system, CGMs can be Open loop or Closed loop
Project Background
• CGM has frequently been prescribed by Endocrinologists. However, most diabetic patients receive their diabetes care through PCPs who often have limited knowledge and experience prescribing, interpreting CGM.
• Many primary care physicians turn to the American Academy of Family Practice (AAFP) website for practice resources. AAFP TIPS™CGM module is a team-based learning tool that was introduced in AAFP website in 2021 and family physicians can use it to implement CGM in their practice.
• Jackson Park Hospital, Family Medicine Clinic was selected by AAFP-National Research Network (NRN) as one of the three pilot sites for evaluation of the module.
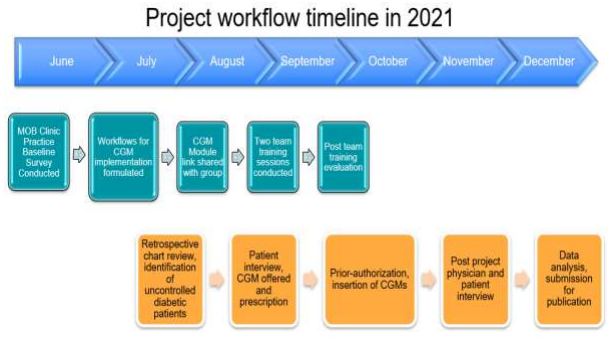
• This project conducted an evaluation of of AAFP TIPS™ CGM module after team training sessions and following the completion of the project. We also developed workflows for implementation in our clinic, recruited patients and taken patient feedback after the project.
.png)

Methods
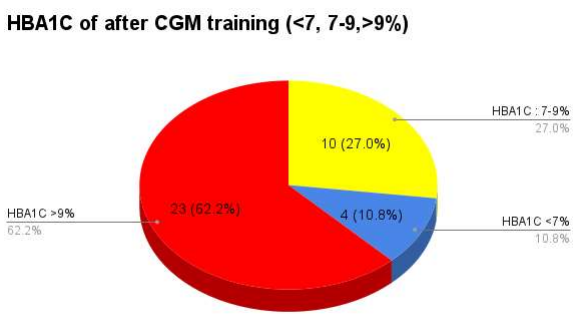
- HBA1C >9% is a widely accepted criterion according to AAFP guidelines to start patients on insulin. This surrogate endpoint was used to identify uncontrolled diabetic patients as possible candidates for CGM prescription. It was also used as a metric for successful glycemic control in our cohort.
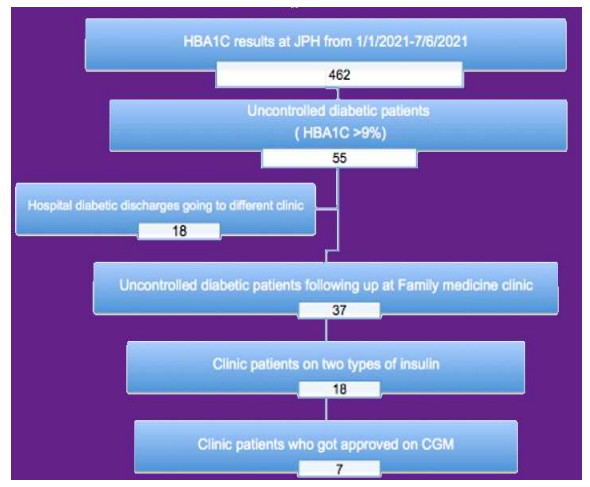
- A retrospective chart review of 462 patients who underwent HBA1c lab work at JPH lab between January, 2021 to June, 2021 was conducted. 37 MOB continuity clinic patients were identified.
- Practice baseline survey was conducted to describe the demographic characteristics of our practice
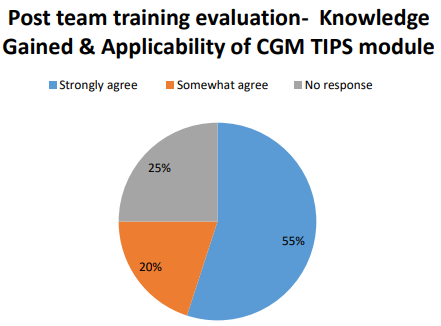
- 2 team training sessions were conducted to disseminate the information about the AAFP CGM TIPS learning module. A post team training survey was conducted to assess the utility, comprehensiveness and applicability of the CGM learning module.
- 4 physician and 5 patients participated in standardized open-ended interview at the end of the project.
- Both qualitative & quantitative methods were utilized to assess patient and physician’s adoption, experience, and feedback with the AAFP TIPS CGM module. Additionally, we used qualitative methods to assess barriers and facilitators for CGM use among patients.
Results
- 40 physicians participated in the post team training survey. 55% participants strongly agreed with knowledge gained and applicability of the module. 20% somewhat agreed and 25% did no response.
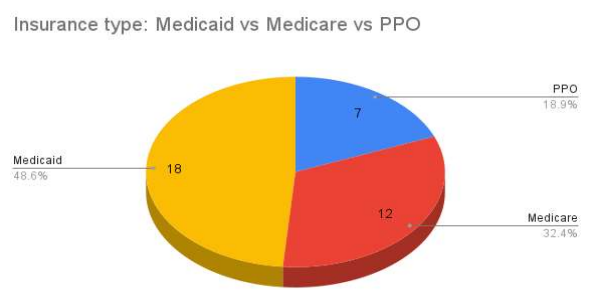
- 37 uncontrolled diabetic patients from MOB continuity clinic were identified to prescribe CGM. After finishing the project in December, 7 patients got approved for CGM. 3 of the approved patients had Medicare, 3 had Medicaid and 1 had PPO based insurance.
- After completion of the project, HBA1C of 10% patients of cohort came under control (9%)
- 4 physicians and 5 patients were interviewed following completion of the project. Patients were generally found enthusiastic to adopt CGM. Barriers such as insurance approval, patient’s understanding level, data interpretation and sharing, DME troubleshooting etc. were identified during the interview.
Discussion
- AAFP TIPS CGM online course would take approximately 2 hours to complete. Its content included Introduction to CGM, Patient identification, billing, coding, CGM data interpretation, EMR charting, clinic workflow management.
- The module did not specifically mention that the patient needs to take at least two types of insulin and check their blood sugar a minimum of four times a day to be approved for CGM. We found that during the preauthorization step of the project.
- 3rd party DME approval companies were involved in the prior-authorization process. A lengthy insurance approval process and third party durable medical equipment (DME) approval communication were identified.
Limitations/barriers
- We could not interview all (18) qualifying patients to identify the barriers for adoption of CGM
- A head-to-head comparison with conventional finger sticks could not be done.
- There was no quantitative comparison about the utility of the CGM TIPS module before and after completion of the project among our providers.
Acknowledgement, dissemination of results
- Funded by AAFP- NRN by an Abbott Educational Grant.
- Co-Principal Investigators: Tamara K. Oser, MD and Sean M. Oser, MD, MPH from University of Colorado, Denver
- Some conclusions derived from this work has been accepted for publication at AAFP- FPM journal “The Last Words” section
- Poster accepted and published on Mount Sinai Research Day,2022
- Poster submitted at AAFP National conference, 2022, awaiting acceptance.