Benefits & Framework of Interprofessional Collaboration in Clinical Practice
Farzana Hoque M.D. MRCP (UK). FACP. FRCP
Associate Professor of Medicine, Saint Louis University School of Medicine, St. Louis, MO, USA
Corresponding Authors: Farzana Hoque M.D.
Correspondence: Saint Louis University School of Medicine, St. Louis, MO, USAIf everyone is moving forward together, then success takes care of itself. – Henry Ford.
Medicine is not a solo performance; it requires collaborative teamwork. While doctors are indeed central to decision-making, collaboration among various healthcare providers ensures that patients receive holistic and well-coordinated care. According to the World Health Organization (WHO), interprofessional collaboration involves health workers from various backgrounds working together with patients, families, and communities to deliver the best possible care. Healthcare is increasingly embracing team-based care to achieve the quadruple aim: improving population health, enhancing the patient experience, reducing healthcare costs, and improving the well-being of healthcare providers and staff.
Keyword: Interprofessional collaboration (IPC) teamwork patient safety patient-centered care nurse-physician relationship
Benefits & Framework of Interprofessional Collaboration in Clinical Practice
Farzana Hoque M.D. MRCP (UK). FACP. FRCP
Associate Professor of Medicine, Saint Louis University School of Medicine, St. Louis, MO, USA
Corresponding Authors: Farzana Hoque M.D.
Correspondence: Saint Louis University School of Medicine, St. Louis, MO, USA
Benefits & Framework of International Collaboration
Extensive research has unequivocally shown that when healthcare providers work together effectively, it yields numerous advantages for patients. These benefits include a notable reduction in preventable adverse drug reactions, improved overall health outcomes with lower rates of morbidity and mortality, and the optimization of medication dosages.1,2,3 Additionally, strengthening a spirit of teamwork among healthcare professionals brings about positive outcomes for the providers themselves, as it helps minimize unnecessary workload and enhances job satisfaction.1
A paper on an interprofessional collaborative practice model at Creighton University School of Medicine ambulatory care center has been published in the Annals of Family Medicine.3 The authors reported significant reductions in emergency room visits, hospitalizations, and hemoglobin A1c levels, attributing these improvements to the implementation of the interprofessional collaborative practice model. This study provides evidence that the utilization of this model can lead to positive outcomes, including improved management of chronic conditions and reduced healthcare utilization.3
- Enhance Patient Safety
Patient safety is of utmost importance, and the medical team employs several practices to enhance it, including daily safety huddles and patient safety and quality meetings. During these meetings, physicians and nursing staff collaborate to identify patients with central lines, foley catheters, and rectal tubes, with a focus on ensuring timely removal. This proactive approach aims to prevent central line-associated bloodstream infections (CLABSI) and catheter-associated urinary tract infections (CAUTI), which pose risks to patient safety. By regularly assessing the necessity of these medical devices and promptly removing them when no longer needed, the medical team reduces the likelihood of infections and associated complications. Regular communication between physician teams and nurses about the management plan reduces the risk of errors and improves efficiency which leads to higher patient satisfaction.
- Safe Transition of Care
Physical and occupational therapists perform essential evaluations during a patient's hospital stay. These assessments are instrumental in determining the appropriate discharge plan for each patient. The insights provided by these evaluations help the inpatient teams to identify patients who can safely return home and those who may require discharge at acute rehabilitation or skilled nursing facilities.
For patients eligible for discharge to their homes, physical therapists and occupational therapists play a vital role in assessing their specific needs. This includes evaluating factors such as the need for home oxygen and determining if any durable medical equipment (DME), such as walkers or canes, is necessary to ensure a safe transition. By carefully assessing and addressing these needs, therapists contribute to patients’ safety during the transition of care. Social workers assist patients to arrange transport if needed and setting up an appointment in the transition of care clinic.
- Foster Health Literacy
When caring for patients with substance use disorders, healthcare providers have the responsibility of educating them about the importance of ceasing illicit drug use. Social workers also provide resources for substance cessation programs directly at the patient's bedside. This proactive approach ensures that patients receive the necessary support and information to initiate their recovery journey.
In cases involving newly diagnosed diabetes patients, those with uncontrolled diabetes, or those experiencing frequent hypoglycemia, healthcare providers consult a diabetic educator. The diabetic educator plays a vital role in providing education on the diabetic diet and the appropriate use of antidiabetic medications, including insulin. This collaborative approach enhances the patients’ understanding of their condition and improves their overall health literacy. By involving multiple healthcare professionals in patient discussions and education at the bedside, there is a higher likelihood of information retention and improved patient outcomes.
- Improve Hospital Throughput
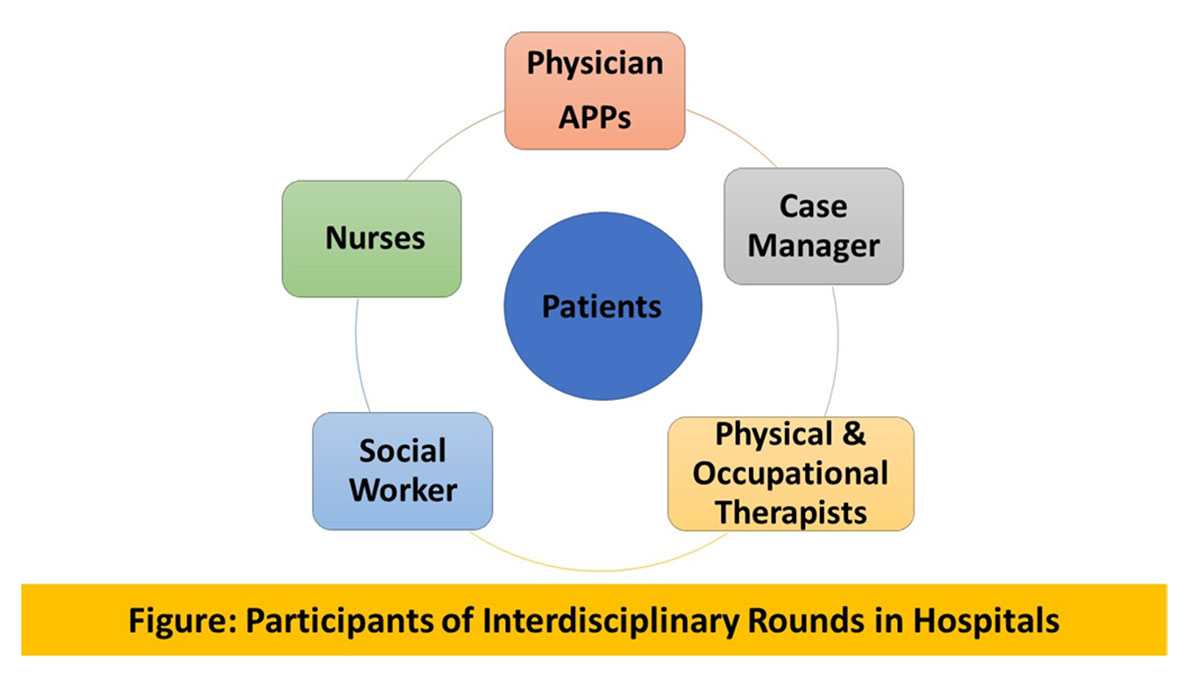
Interdisciplinary rounds bring together healthcare professionals from different disciplines, including doctors, nurses, pharmacists, social workers, therapists, and others involved in a patient's care. Numerous studies have indicated that interdisciplinary rounds have a positive impact on hospital throughput, which refers to the efficiency and flow of patients through the healthcare system. 2,3 Interdisciplinary rounds focus on discharge planning from an early stage of a patient's hospital stay.
This proactive approach helps in streamlining the discharge process, identifying potential barriers, and arranging for necessary support services to ensure safe discharge. Interdisciplinary rounds optimize resource utilization and create an efficient workflow that reduces costs and improves staff satisfaction. 2,3
- Promote Medication Adherence
Direct bedside delivery of medications before discharge eliminates the need for patients to visit the pharmacy after discharge and ensures they have all the necessary prescribed medications readily available at home. This service enhances patient convenience and promotes adherence to their medication regimen. Additionally, involving pharmacists in counseling patients about their newly prescribed medications like anticoagulation can improve patients’ understanding of the indications and proper usage of their medications. This increased awareness reduces the likelihood of medication errors and enhances patient safety.
- Holistic Approach to Patient Care
Having firsthand experience as a patient in a hospital allows one to appreciate the overwhelming nature of the experience. For patients who lack social support or find themselves in emotional distress after receiving a new diagnosis, bedside prayers facilitated by the pastoral care team offer patients an opportunity to find solace and express their feelings and personal stories and promoting comfort. In addition, there is a growing recognition of the benefits of incorporating service animals and music therapy for interested patients. These initiatives contribute to an environment that promotes healing, emotional well-being, and a greater sense of comfort during their hospital stay.
Potential Obstacles to international Collaboration
Each team member in the healthcare setting has their own goals and priorities, which can make it difficult to work together effectively.5 One of the main challenges healthcare professionals face when trying to collaborate is the lack of clear leadership and role definition.5 To overcome this obstacle, it's crucial to establish clear roles and responsibilities for everyone involved. It's also important to recognize and value everyone’s contributions so that all team members feel engaged and motivated to work together. The focus should be on the success of the entire team, as this will lead to the best performance and ultimately result in improved outcomes for patients.1,5 Team diversity is an asset because it brings together individuals with different perspectives, enabling a wide range of viewpoints and fostering innovation and effective problem-solving.
Conclusion
The provision of safe and patient-centered care is at the core of our mission. The evolving healthcare landscape has highlighted the limitations of individual practitioners in meeting the complex needs of diverse patients. Therefore, interprofessional collaboration among healthcare professionals is imperative. Through collaboration, we can harness the diverse expertise and perspectives of a range of professionals to achieve higher patient satisfaction and optimize healthcare delivery.
- Bosch B, Mansell H. Interprofessional collaboration in health care: Lessons to be learned from competitive sports. Can Pharm J (Ott). 2015;148(4):176-179.
- Green BN, Johnson CD. Interprofessional collaboration in research, education, and clinical practice: working together for a better future. J Chiropr Educ. 2015;29(1):1-10. doi:10.7899/JCE-14-36
- Thomas P. Guck, Meghan R. Potthoff, Ryan W. Walters, Joy Doll, Michael A. Greene, Todd DeFreece. The Annals of Family Medicine Aug 2019, 17 (Suppl 1) S82.
- Interdisciplinary rounds reduced hospital stay and costs and improved staff satisfaction. Evidence-Based Nursing 1999; 2:56.
- Jabbar S, Noor HS, Butt GA, et al. A Cross-Sectional Study on Attitude and Barriers to Interprofessional Collaboration in Hospitals Among Health Care Professionals. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2023;60. doi:10.1177/00469580231171014