Ultrafast and simple acute ischemic stroke therapy based on evidence; potential for cost reduction and global access
Yahia Lodi , Aria Soltani , Rohan Arora
1Neurology, Neurosurgery & Radiology, Upstate Medical University and UHS-Hospitals, Johnson City, NY
2Department of Neurology, Zucker School of Medicine at Hofstra/Northwell, New York
The recent impact of improvement in the treatment of acute ischemic stroke (AIS) resulted in a reduction in death and an improvement in outcomes, especially in developed countries. The results of groundbreaking positive randomized controlled trials have revealed that patients with large vessel occlusion (LVO) treated with endovascular mechanical thrombectomy (EVMT) compared with standard treatment are associated with significantly higher functional outcomes. Current evidence also confirmed that the early positive outcomes of EVMT continue to persist for stroke patients with LVO even if the mechanical perfusion therapy extends up to 24 hours of symptoms, including those with wake-up stroke. The evidence suggests that for every two patients treated with EVMT, one patient can be saved, which is the highest evidence in the medicine surpassing acute myocardial infarction and other acute lifesaving therapies. Based on this evidence, local, national, and international organizations have updated the guidelines in the treatment of AIS, which have remarkably strengthened the process, pathways, and standards for acute ischemic stroke management in developed countries. However, not much progress has been made in developing and third-world countries, including Bangladesh, for stroke therapies because of cost and affordability, and there are no third-party payers. Most recent trials have further identified that stroke patients with LVO and a large core volume can be treated with endovascular perfusion therapy in conjunction with standard treatment, which is associated with significantly better compared to standard treatment only. Recent trials have also demonstrated that stroke patients undergoing EVMT with or without thrombolytic have equal functional outcomes. Additional evidence suggests that non-disabling stroke patients treated with dual antiplatelet agents have equal functional outcomes with less bleeding risk compared to intravenous thrombolysis. This evolving evidence has provided us with opportunities to simplify the algorithm and treatment of acute ischemic stroke, which not only will cut down time by eliminating unnecessary steps and redundant therapies but also will reduce healthcare costs and improve global access, especially in countries where patients bear the costs. In this review, the author presents real-life stroke patients treated based on recent evidence and provides a simple and swift algorithm that potentially may reduce the time for perfusion therapy and make the treatment affordable globally, including in developing countries like Bangladesh.
Ultrafast and simple acute ischemic stroke therapy based on evidence; potential for cost reduction and global access
Yahia Lodi , Aria Soltani , Rohan Arora
1Neurology, Neurosurgery & Radiology, Upstate Medical University and UHS-Hospitals, Johnson City, NY
2Department of Neurology, Zucker School of Medicine at Hofstra/Northwell, New York
INTRODUCTION:
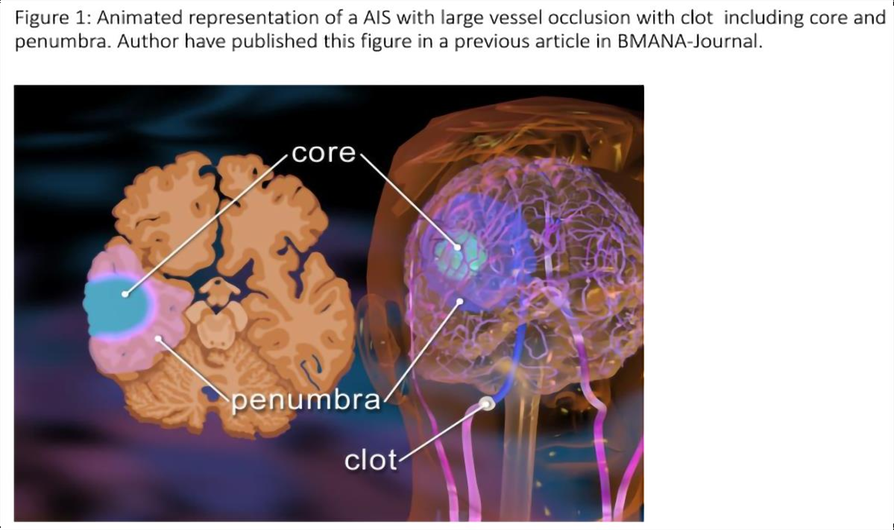
The risk of death of millions of vulnerable brain tissue is imminent in acute ischemic stroke (AIS) with ongoing ischemia, especially in strokes with LVO. An ultrafast triage and early perfusion therapy may be necessary for good function outcomes and the prevention of long-term disabilities. AIS develops when a blood vessel is occluded by a thrombus from within or by a thrombus travelling from the other part of the body, mainly from the heart impairing the blood flow and oxygen supply to the area of the brain supplied by that particular blood vessel. The center of the area of the brain suffering from oxygen is called the core, where the oxygen supply falls below the threshold of brain cell survival. The areas around the core are called the penumbra, where the cells are suffering from impaired oxygen supply but are still salvageable by restoration of blood flow (Figure 1). In AIS, the occluded blood vessels may be large, medium, or small (Figure 2), but all require immediate triage and perfusion treatment for better outcomes. The intravenous (IV) thrombolytic (tPA) was first introduced in 19951 for AIS patients presenting with disabling stroke with 3 hours of symptoms onset. The tPA was subsequently approved up to 4.5 hours both in the United States and Europe.2,3 In some instances, tPA could be utilized for up to 9 hours in specific selected patients based on perfusion imaging when no endovascular mechanical thrombectomy (EVMT) is available.4 AIS patients with large vessel occlusion (LVO) have disproportionally poor outcomes compared to non-LVO.5 The positive results of groundbreaking randomized control trials6-13 of acute ischemic stroke with large vessel occlusion (LVO) allow patients to receive perfusion therapy within 24 hours of onset, and which is also considered as a standard of care. These novel innovations and initiatives have significantly improved stroke care with the reduction of mortality and morbidity with better outcomes. Presenting stroke symptoms depends on the impaired territory of the brain supplying a specific blood vessel either in the anterior or in the posterior circulations (Table 1). Available data from these trials also have given us the foundations of clinical signs and symptoms that best correlate with LVO in the anterior circulation. Significant focus has been given to the early identification of AIS with LVO and faster therapy. There are numerous field AIS scales which have been validated in the clinical practice for AIS with LVO.14-17 Emergency medical service (EMS) uses these field scales of LVO for faster triage and appropriate destination. Subsequently, EMS brings the suspected LVO patients to the designated stroke center capable of EVMT for early perfusion therapy. Unfortunately, in the emergency department (ER) and hospital, neurological examinations are again being repeated using NIHSS, which takes longer time, and many of the components of NIHSS do not represent LVO, leading to missing the opportunity.
Additionally, after the lengthy NIHSS evaluation, patients are sent for multiple images, including computed tomographic angiography (CTA), computed tomography (CT) with Alberta stroke program early CT (ASPECT), and computed tomographic perfusion (CTP) leading to further delay in the definitive perfusion therapies with the addition of more cost in the triage of the patient, which could be avoided based on the most recent evidence. 18,19 From a healthcare institution's perspective, the implementation of such care, the healthcare system must be resourceful and financially sound to process the complex triage process followed by performing a series of images with rapid interpretations, which adds additional layers of delays and financial burden. Based on emerging evidence, 18,19 many images such as CTA, CTP, magnetic resonance imaging (MRI), magnetic resonance imaging perfusion (MRP), or steps that are usually taken for the triage may not be necessary to provide early or late perfusion therapy without harm. These additional steps not only cause delays but also cause redundancy and significantly increase the healthcare cost. In regard to treatment for LVO, these complex processes may create a challenging environment when patients have to pay out-of-pocket, which is the fact for most of the countries in the world where there are no third parties to pay for these redundant steps, including images and combination therapies.
Unfortunately, patients have to choose one over the other because of affordability as well as availability. Recently, the author has introduced a new in-hospital/ER acute ischemic stroke with LVO scale for the anterior circulation, which has been validated with CTA, named GWNS stroke scale. 20 The GWNS stroke scale could be easily performed in 3 minutes and would predict LVO better than a lengthy NIHSS. In this review article, authors have presented a few AIS patients who were triaged using the GWNS acute stroke scale and treated them with the most recent evidence based on the RCT. The latest RCTs for LVO 21 and non-LVO 22,23 may have shaded some lights to guide us to make decisions in those circumstances related to cost, affordability, and availability that have global implications without impairing outcome.
The first objective of this review is to explain to the readers that an AIS patient could be triaged and treated as an early or late arrival for perfusion therapy using a simple and economical pathway based on the evidence without sacrificing the outcomes. Secondly, this review clarifies the rationale of choosing a particular triage and treatment option over others for a specific stroke patient of a particular clinical scenario. Finally, the authors provide their recommendations for faster and affordable acute ischemic stroke therapies using a simple and swift triage and treatment algorithms for possibilities of regional and global access.
.png)
METHODS:
This is a review article that has included most of the published randomized control trials of AIS with LVO and non-LVO. The review also includes the most recent trials for early and late arrival AIS with LVO that have included patients with large volume strokes, and the selection of patients was based on CT, ASPECT, or perfusion imaging. The review article included studies where simple CT, ASPECT imaging-based selection of patients were compared with advanced imaging modalities, including CTP or MRI. For a better understanding of the readers, the review article has presented a few index patients who were treated based on the recent evidence and used them as references in the article for further reviews and discussions.
Review of literature using real cases:
In our review, the first reference patient is an 85-year-old man with a history of hypertension, and hyperlipidemia, who presented to the hospital with NIHSS of 5, GWNS stroke scale of 2 20 , and last known normal (LKN) 4 1/2 hours ago, and his CT Alberta stroke program early CT (ASPECT) was 10. 24 The treatment options were discussed with the patient and the family. Treatment options are intravenous tissue plasminogen activator (TPA), intravenous TNK, and loading doses of aspirin and clopidogrel. The Family also wanted to know the natural history of the recovery for a patient with a small NIHSS. 1,3 The natural history was explained to the patient stating that most of the patients with NIHSS less than 6 do better but there is evidence that may do better with thrombolytic, however there is a chance of intracranial hemorrhage (ICH) among patients receiving thrombolytic. The patient's family wanted to explore more about giving aspirin and Plavix based on the most recent trial. 22,23 The Patient's family was told that this study was performed in China, which has demonstrated equal benefit with aspirin and clopidogrel versus intravenous TPA with less asymptomatic hemorrhagic transformation. The patient was loaded with 4 baby aspirin and 300 mg of clopidogrel. The patient's remaining management was followed based on the American Heart Association guidelines. The patient's symptoms completely resolved and NIHSS became 0. The patient’s stroke workup demonstrated the right internal carotid artery (ICA) with more than 70% stenosis. The patient was offered ICA revascularization options and underwent successful stenting of the right ICA with an embolic protection device (AHA guidelines). The patient was discharged home with NIHSS zero and a modified ranking score (mRS) of 1, which is at his baseline. Our next reference patient is a 43-year-old woman with a history of hypertension and hyperlipidemia who presented with left-sided ataxic hemiparesis, including sensory symptoms and dysmetria, with NIHSS of 5 and LKN 4 hours ago, with presenting ASPECT of 10. It was felt to be related to the small vessel disease and maybe benefited from aspirin clopidogrel over IV thrombolytics. The patient was offered both treatment options and chose aspirin and clopidogrel. The patient's symptoms resolved, and MRI demonstrated a right subcortical lacunar stroke. The patient’s stroke workup was negative except for risk factors of hypertension, hyperlipidemia, diabetes, and smoking. The patient was counseled on the stroke risk factors, including smoking cessation and a healthy diet with physical activity options. She was prescribed atorvastatin and antihypertensives and scheduled to have a follow-up with a stroke specialist. Our third reference patient was last known normal 2 hours ago, presented with right facial droop, right pronator drift with word finding problem, and NIHSS of 5 GWNS stroke scale 2.20. The Patient did not have any large vessel occlusion, and we offered thrombolytic. The patient was reluctant; however, we have given the evidence that the patient might be benefited. The patient received the thrombolytic, and the symptoms resolved in 12 hours. She was in the critical care unit. The cause of the stroke was intermittent atrial fibrillation. The patient was sent home with apixaban 5 mg two times a day with all risk reduction strategies based on AHA guidelines.25
In this review, the 4th reference patient is a 65-year-old man with a history of AF presented with an AIS, and his field FAST-ED was 4 by EMS, and the patient was brought to the hospital. The patient has right gaze with left hemiparesis and neglect with GWNS stroke scale 420 and NIHSS 19 . The patient’s CT ASPECT was 9. The patient immediately received IV TPA1,3,24 and was brought to the interventional suite for mechanical thrombectomy, bypassing CT angiogram and CT perfusion.18,21 The patient received full perfusion within 3 hours. Repeat CT head no ICH, but small basal ganglia stroke. His NIHSS became 0 in 48 hours. The patient was started on apixaban 5 mg two times a day with secondary risk factor reduction, including Stroke education. Our 5th patient is a 48-year-old man, educated, self-employed, and self-paying, presented with right-sided gaze, left-sided hemiparesis, and neglect, presented within 11/2 hours of symptoms, GWNS stroke scale 4 indicating AIS with LVO. The patient’s wife was also with him. The patient and family made it clear that he has a large medical bill, and he would like to choose the best option for his treatment. The patient was offered IV thrombosis followed by mechanical thrombectomy. After reviewing the risks and benefits, including cost and most current evidence,26,27 the patient wanted EVMT without thrombolytic. Additionally, the author had a pilot trial
of primary EVMT without IV tPA that demonstrated similar results to the most recent RCT.26,27 The patient was told that the chances of complete perfusion may be less if no tPA is chosen, but, there were no differences in outcomes.21 However, it was made clear to the patient that there is no guarantee of outcomes irrespective of his decisions. The patient received 300 mg aspirin rectally and underwent EVMT with a stent retriever device, resulting in complete perfusion and became normal in 24 hours. He was discharged home in 48 hours with apixaban 5 mg two times a day with all stroke risk factor modification strategies based on AHAS guidelines.25 Patient went to work in 7 days and achieved his baseline mRS of 0. The next reference patient that we have used for the review of literature is a 78-year old woman with a history of tremors and baseline mRS of 2, who was last known to be normal 12 hours ago. The patient was found on the floor with left gaze, right hemiparesis, and aphasia; GWNS stroke scale of 3.20. The Patient was brought to the emergency department, where she was found to have NIHSS 25 and GWNS scale of 3 and required immediate intubation because of her airway. The CTA demonstrates left M2 occlusion, and the ASPECT score was 9 and the patient underwent immediate EVMT without CT perfusion18,21 after receiving 300 mg rectal aspirin. The patient achieved TICI3 perfusion (Fig1), and her 24-hour CT head demonstrates no large stroke. The patient was started on apixaban 5 mg two times a day. The patient was extubated in 48 hours, and NIHSS became 0. She required inpatient rehab and achieved her baseline mRS 2 at 90 days.
.png)
.png)
.png)
.png)
The next index patient we have chosen for the review of the literature was a 50-year-old woman admitted to stroke service with left MCA non-LVO stroke beyond the thrombolytic window. The patient was placed on both aspirin and clopidogrel, and NIHSS improved from 9 to 3 on day 3. On day 4, the patient was found to have right gaze, left hemiparesis, and right neglect (GWNS stroke scale 3), NIHSS 19, ASPECT9, and CTA demonstrated right MCA distal branch occlusion. The patient underwent EVMT without CTP.18,21 The Patient achieved TICI 3 perfusion (Fig 2), and her NIHSS went to 3 in 24 hours and 1 on day 5, despite density on the CT head (Fig 2).
The patient was sent to rehab, and her mRS became 2 in 30 days. The final reference patient used for the review article is a 55-year-old woman who suddenly developed left gaze deviation, right-sided weakness, and aphasia in a nonstroke-designated rural hospital, LKN, 30 minutes ago. The patient was triaged and recommended to be brought to a stroke hospital. Because of the rural ambulance shortage, the patient was airlifted and brought to the hospital 2 hours after her stroke onset. Upon arrival at the endovascular center, the patient's GWNS stroke scale was 320, and NIHSS 25 required immediate endotracheal intubation. Plans were to just perform CT followed by IV TPA based on ASPECT and immediately to NES for faster EVMT. The ASPECT was 5, and he was not a candidate for intravenous thrombolytic and underwent EVMT without any advanced imaging.14,18,21 Angiography demonstrated left ICA-T occlusion, and TICI 3 perfusion was achieved with 2 passes using a balloon guide, intermediate catheter, and 4 mm x 40 mm stent retriever (Figure 3A). It was discovered after the thrombectomy that the patient was on apixaban (Eliquis) for clots in her kidney, and she ran out of her medicine 3 days ago. The follow-up two CT heads in 6-hour intervals (Fig 3B) didn’t demonstrate any perfusion-related intracranial hemorrhage. Considering the patient history of multiple thrombo-embolic events and prevention of potential subsequent events, it was decided to start intravenous heparin to keep the apparent partial thromboplastin (aPTT) 1.5 to 2 times her baseline aPTT. The patient baseline aPTT was 28, and the aPTT target was 45 to 55. The 24-hour follow-up CT head after initiation of IV heparin revealed no ICH (Fig 3B). After 5 days, the IV heparin was switched to apixaban. The patient improved and went to inpatient rehabilitation.
Discussion:
Our real-time stroke patients chosen for this review article had low to high NIHSS and have presented in the early or the late stage of stroke and underwent interventions based on the recent trials, guidelines, and publications resulting in good outcomes. Additionally, our treatment strategies have not only simplified the stroke triage and treatment algorithms with the initiation of early perfusion therapy but also reduced the healthcare system resource utilization and provided an option for a patient who pays out of pocket. The authors have linked the real stroke patients' triage and treatment scenarios with currently available publications to make this review interactive and interesting. In a recent trial,22 AIS patients with NIHSS 5 or less were randomized to receive IV tPA or loading dose of 300 mg clopidogrel and 100 mg aspirin, followed by 75 mg of clopidogrel and 100 mg aspirin daily for 14 days. There was no significant difference22 in regard to favorable function outcomes (mRS 0-1) between these two arms at 90 days as a primary outcome: the aspirin-clopidogrel group (91.6%) achieved a favorable functional outcome at 3 months versus 85 (78.0%) in the alteplase group (OR 4.463, 95%CI 1.708– 11.662, p=.002). Asymptomatic ICH occurred in 0.8% of patients who received aspirin-clopidogrel, as compared with 3.7% of patients in the alteplase group (p=.030), meaning the alteplase group had a higher incidence of AICH than the dual antiplatelet group. Additionally, in the original NINDS and ECASS trills, patients with minor disabling stroke patients were excluded.
The PRISMS23 trial (aspirin 325 mg plus IV placebo vs IV tPA and oral placebo) also have demonstrated no significant difference in clinical outcome in regard to 90 days mRS; 78.2%in the alteplase group vs 81.5% in the aspirin group achieved a favorable outcome (adjusted risk difference, −1.1%; 95% CI, −9.4% to 7.3%). In this trial, 5 alteplasetreated patients (3.2%) vs 0 aspirin-treated patients had sICH (risk difference, 3.3%; 95% CI, 0.8%-7.4%). In our reviews, the first reference patient presented with minor non-disabling stroke, NIHSS 5 and older than 85, who have chosen not to receive thrombolytic but antiplatelets as an alternative option and have achieved good functional outcomes. The 2nd reference patient also presented with non-disabling lacunar stroke with NIHSS 5 and has chosen the alternative option of acute antiplatelets instead of thrombolytic, resulting in a good outcome. The alternative option of dual antiplatelets was offered based on the most recent RCT evidence22,23 with a modified dose of aspirin 324 mg instead of 100 mg.
In regard to the cost and resources for developed countries, both our patients have saved significant health care costs and allocation of resources, including not requiring critical care stay and potential additional stay in the critical care unit and hospital. If these two patients had received TPA, they should have been required to be monitored in the critical care unit as a standard of care after thrombolytic and potentially would have stayed more days in the critical care unit or hospital if they had developed asymptomatic or symptomatic ICH following thrombolytic, occupying the rare resources for those who are still waiting in the ER or transferred out of the community creating significant inconveniences and burden for the patient and their family. Hypothetically, in regard to the individual, regional, and global economic impact where, a patient with out-of-pocket expenses will have to spend remarkably less if dual antiplatelet is used instead of IV tPA. In many third-world countries, tPA is expensive, not available, and substituted with alternative thrombolytics may lead to more complications and fewer benefits. Additionally, the dual antiplatelet options would also simplify the stroke system care and access, as the aspirin and clopidogrel are very affordable and readily available all over the world, including in third-world countries.
In this review, the 3rd reference patient received IV thrombolytic despite having a low NIHSS as the patient had disabling stroke symptoms and achieved a good outcome. Additionally, the patient had a history of atrial fibrillation associated with embolism likely, justifying our decision 1-3
The 4th reference patient in our review presented with suspected right-sided LVO based on FAST-ED and had high NIHSS with cortical representation; right gaze, left hemiparesis, dysarthria, and neglect with a GWNS scale of 4.20 Patient ASPECT was 9 and received tPA, and underwent EVMT without advanced imaging. Based on FAST-ED LVO validation with NIHSS 29 as well as GWNS in hospital stroke scale, 20 this patient has a very high likelihood of having LVO, making it justifiable to take the patient for definitive perfusion therapy. This strategy simplified the process and avoided the delay and unnecessary intravenous 100 ml contrast and exposure to additional radiation. Additionally, multiple RCTs have demonstrated that IV tPA with EVMT with early perfusion has a better outcome.
The 5th reference patient in the review poses a real challenge as he is self-employed and bears the medical cost out of pocket. This patient had a similar clinical scenario to our previous case and with suspected LVO and only had CT with ASPECT 10. The patient has chosen EVMT alone instead of IV tPA plus EVMT after informed consent. The justification and agreement with the patient's decision are based on the most recent publication in NEJ26 as well as JAMA.27 In endovascular therapy with or without IV tPA in acute ischemic stroke 26 , 327 patients were assigned to the thrombectomy-alone group, and 329 were assigned to the combination therapy group. Endovascular thrombectomy alone was non-inferior to combined intravenous alteplase and endovascular thrombectomy with regard to the 90 days mRS (adjusted common odds ratio, 1.07; 95% confidence interval, 0.81 to 1.40; P=0.04 for noninferiority) but was associated with lower percentages of patients with successful reperfusion before thrombectomy (2.4% vs.7.0%) and overall successful reperfusion (79.4% vs. 84.5%). Mortality at 90 days was 17.7% in the thrombectomy-alone group and 18.8% in the combination therapy group. The study concluded that in Chinese patients with AIS from LVO, EVMT alone was non-inferior with regard to functional outcome, within a 20% margin of confidence, to endovascular thrombectomy preceded by intravenous alteplase administered within 4.5 hours after symptom onset. In Skip randomized clinical trial 27 , favorable outcomes occurred in 60 patients (59.4%) in the mechanical thrombectomy alone group and 59 patients (57.3%) in the combined intravenous thrombolysis plus mechanical thrombectomy group, with no significant difference between-group in regards to 90-day mRS (difference, 2.1% [1-sided 97.5% CI, -11.4% to ∞]; odds ratio, 1.09 [1-sided 97.5% CI, 0.63 to ∞]; P = .18 for noninferiority) with no differences in mortality. Any intracerebral hemorrhage was observed less frequently in the mechanical thrombectomy alone group than in the combined group (34 [33.7%] vs 52 [50.5%]; difference, - 16.8% [95% CI, -32.1% to -1.6%]; odds ratio, 0.50 [95% CI, 0.28 to 0.88]; P = .02). Symptomatic ICH was not significantly different between groups (6 [5.9%] vs 8 [7.7%]; difference, -1.8% [95% CI, -9.7% to 6.1%]; odds ratio, 0.50 [95% CI, 0.28 to 0.88]; P = .02). Symptomatic ICH was not significantly different between groups (6 [5.9%] vs 8 [7.7%]; difference, -1.8% [95% CI, -9.7% to 6.1%]; odds ratio, 0.75 [95% CI, 0.25 to 2.24]; P = .78). The study concluded that among patients with AIS with LVO, EVMT alone, compared with combined IV tPA plus EVMT, failed to demonstrate noninferiority regarding favorable functional outcome.
In regard to the simplicity and stroke system of care, direct EVMT will simplify the triage and the treatment by cutting extra steps that would have been required in the process and policies of IV tPA administration. Our index patient was taken directly to NES without IV tPA. Additionally, we have not performed any advanced images, such as CTA and CTP leading to much simplicity in the process and a significant reduction of precious time. If we look at the cost, this patient has avoided the out-of-pocket cost of tPA and advanced images and still has achieved a good outcome. In regard to global implications, in most countries, there are no third-party; patients and their families bear the health care cost upfront. Therefore, using direct EVMT without tPA would have made the treatment accessible and affordable. The author would like to emphasize that in AIS with LVO, EVMT is the driver of clinical outcome,26,27 not IV tPA, but, it is an adjunct. Therefore, unnecessary waiting and losing time for IV tPA administration prior to EVMT should be avoided, especially when it is not clear if the patient is or is not a candidate for thrombolytic. The author believes that this strategy will help improve access to perfusion therapies for stroke victims with LVO in countries where the patient or institution has to pay on their own, cutting the cost in half without impairing outcomes and not having to choose between thrombolytic and EVMT.
For the final reference patient of our review article, the presenting GWNS and NIHSS were indicative of an LVO with large territory ischemia. Additionally, patient’s repeat CT, ASPECT reduced to 5 in 2 hours, indicating the presence of poor collateral or poor cerebral reserve. Because of her rapidly declining ASPECT as well as recent evidence,14,19 we have avoided advanced imaging, including CTA and CTP, and initiated early perfusion therapy resulting in complete reperfusion. In support to our simplified strategy, in a recent study,15 outcomes of patients after EVMT selection based on CT/ASPECT, CTA/CTP, or MRI/MRI perfusion were evaluated and found to have no significant difference among the groups in regard to the functional outcome or risk of ICH.
Patients selected based on MRI/MRI perfusion did poorly compared to ASPECT on CT head.
The explanations are very simple: the initiation, screening, and performing MRI/MRP required time, resulting in losing precious penumbra, which is not only impractical but also should be avoided. In regard to CTA/CTP, CTA will need time for the administration of 100 ml of contrast as well as its interpretation, requiring additional time. It is reasonable to bring this patient directly to NES, as the patient is already in an endovascular center and the surgeon is ready. Therefore, an extra step was avoided. Regarding CTP, CTP requires more time delays in perfusion therapy in addition to exposure to more radiation. The CTP is also dependent on the timing of IV admiration of contrast and patient factors, including hemodynamic status, which may lead to improper accusation and interpretation. Based on the above, performing CTA/CTP may not contribute significantly, but it definitely will cost more brain cells and health care burden for the patient and for the health system. In another large cohort study,14 more than 1 in 5 patients presenting with an ASPECTS of 2 to 5 achieved 90-day functional independence after EVMT. A favorable outcome was nearly 5 times more likely for patients with low ASPECTS who had successful recanalization. The association of low ASPECTS with 90-day outcomes did not differ for patients presenting in the early vs. extended EVMT window. In this study,19 213 patients [9.1%] had an ASPECTS of 2-5). At 90 days, 47 of the 213 patients (22.1%) with an ASPECTS of 2 to 5 had a modified Rankin Scale score of 0 to 2 (25.6% [45 of 176] of patients who underwent successful recanalization [modified Thrombolysis in Cerebral Ischemia score ≥2B] vs 5.4% [2 of 37] of patients who underwent unsuccessful recanalization; P = .007). Therefore, we initiated early perfusion therapy and achieved TICI 3 perfusion.
The most recent SLECT2 trial also shed light on the outcomes of patients with low ASPECT scores. The SELECT2 is a prospective, 1:1 ratio to endovascular thrombectomy plus medical care or to medical care alone, open-label, adaptive international trial involving patients with stroke due to occlusion of the ICA-Terminus or the first segment of MCA to assess endovascular thrombectomy within 24 hours after onset. Eligibility criteria were a large ischemic-core volume, defined as an Alberta Stroke Program Early Computed Tomography Score of 3 to 5 or a core volume of at least 50 ml on computed tomography perfusion or diffusion-weighted magnetic resonance imaging. Patients assigned with EVMT plus medical management have significantly better outcomes compared to medical management only (20% of the patients in the thrombectomy group and 7% in the medical-care group had functional independence (relative risk, 2.97; 95% CI, 1.60 to 5.51) without any differences in mortality. The generalized odds ratio for a shift in the distribution of modified Rankin scale scores toward better outcomes in favor of thrombectomy was 1.51 (95% confidence interval [CI], 1.20 to 1.89; P<0.001). The SELECT2 trial results will help us to recruit AIS with large volume stroke and LVO for EVMT perfusion therapy, who otherwise would have been treated medically, only missing the opportunities of achieving good functional outcomes.
Conclusions: In conclusion, the evidence suggests that minor non-disabling stroke patients could be treated with a loading dose of aspirin and clopidogrel instead of intravenous thrombolytic therapy, achieving the same functional outcome with less chance of intracranial hemorrhage. In the review, we have demonstrated that AIS patient could be triaged immediately using an LVO stroke20 scale and bought directly to the EVMT room after a simple CT with ASPECT without advanced imaging for early perfusion therapy. Emerging data suggest that AIS with LVO within 4.5 hours of symptoms onset achieves a similar outcome if treated directly with EVMT compared to intravenous thrombolytic followed by EVMT, which we have demonstrated in our index patients. We have also reviewed that for the early or late selection of patients for perfusion therapy with EVMT, a plain CT with ASPECT score is as good as performing advanced imaging with CTP and MRI with perfusion without harm. Most recent evidence suggests that AIS patients with LVO and a large volume stroke (50 ml and higher) treated with EVMT in conjunction with standard treatment do significantly better compared to standard medical management. Finally, we have discussed that an AIS patient with LVO and presenting CT ASPECT score as low as 2 benefits from EMVT without increasing chances of symptomatic intracranial hemorrhage. Based on the above evidence, we have simplified the algorithm in the treatment of AIS patients for early perfusion therapy, which will make the triage and treatment process swift, leading to improved outcomes. Additionally, these strategies will further simplify global access to AIS therapies by cutting down the cost with redundant triage, imaging, and treatment. We are presetting the current complex and comprehensive triage algorithms that are utilized for the treatment of AIS (Table 1). The author is also proposing the simplest and swift algorithm, which could be utilized regionally and globally based on regional and global accessibility and affordability (Table 2). Therefore, the treating stroke team and the patient may choose the best option based on the personal, local, and regional affordability and availability of resources without sacrificing the care and outcomes.
.png)
.png)
1. National Institute of Neurological D, Stroke rt PASSG. Tissue plasminogen activatorfor acute ischemic stroke. N Engl J Med. Dec 14 1995;333(24):1581-7. doi:10.1056/NEJM199512143332401
2. Lansberg MG, Bluhmki E, Thijs VN. Efficacy and safety of tissue plasminogen activator 3 to 4.5 hours after acute ischemic stroke: a metaanalysis. Stroke. Jul 2009;40(7):2438-41. doi:10.1161/STROKEAHA.109.552547
3. Hacke W, Kaste M, Bluhmki E, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. Sep 25 2008;359(13):1317-29. doi:10.1056/NEJMoa0804656
4. Ma H, Campbell BCV, Parsons MW, et al. Thrombolysis Guided by Perfusion Imaging up to 9 Hours after Onset of Stroke. N Engl J Med. May 9 2019;380(19):1795-1803. doi:10.1056/NEJMoa1813046
5. Malhotra K, Gornbein J, Saver JL. Ischemic Strokes Due to Large-Vessel Occlusions Contribute Disproportionately to Stroke-Related Dependence and Death: A Review. Front Neurol. 2017;8:651. doi:10.3389/fneur.2017.00651
6. Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the Merci Retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non- inferiority trial. Lancet. Oct 6 2012;380(9849):1241-9. doi:10.1016/S0140-6736(12)61384-1
7. Sarraj A, Hassan AE, Abraham MG, et al. Trial of Endovascular Thrombectomy for Large Ischemic Strokes. N Engl J Med. Apr 6 2023;388(14):1259-1271. doi:10.1056/NEJMoa2214403
8. Almallouhi E, Al Kasab S, Hubbard Z, et al. Outcomes of Mechanical Thrombectomy for Patients With Stroke Presenting With Low Alberta Stroke Program Early Computed Tomography Score in the Early and Extended Window. JAMA Netw Open. Dec 1 2021;4(12):e2137708. doi:10.1001/jamanetworkopen.2021.37708
9. Lodi YH, Bowen A, Soltani A. Gaze Weakness Neglect and Speech: An Acute Stroke Scale for Large Vessel Occlusion in the Emergency Department for Faster Treatment. Medical Research Archives. 2023;11(5)doi:10.18103/mra.v11i5.3865
10. Nguyen TN, Abdalkader M, Nagel S, et al. Noncontrast Computed Tomography vs Computed Tomography Perfusion or Magnetic Resonance Imaging Selection in Late Presentation of Stroke With Large-Vessel Occlusion. JAMA Neurol. Jan 1 2022;79(1):22-31. doi:10.1001/jamaneurol.2021.4082
11. Lan L, Rong X, Shen Q, et al. Effect of alteplase versus aspirin plus clopidogrel in acute minor stroke. Int J Neurosci. Sep 2020;130(9):857-864. doi:10.1080/00207454.2019.1707822
12. Khatri P, Kleindorfer DO, Devlin T, et al. Effect of Alteplase vs Aspirin on Functional Outcome for Patients With Acute Ischemic Stroke and Minor Nondisabling Neurologic Deficits: The PRISMS Randomized Clinical Trial. JAMA. Jul 10 2018;320(2):156-166. doi:10.1001/jama.2018.8496
13. Pexman JH, Barber PA, Hill MD, et al. Use of the Alberta Stroke Program Early CT Score (ASPECTS) for assessing CT scans in patients with acute stroke. AJNR Am J Neuroradiol. Sep 2001;22(8):1534-42
14. Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. Mar 2018;49(3):e46-e110. doi:10.1161/STR.0000000000000158
15. Yang P, Zhang Y, Zhang L, et al. Endovascular Thrombectomy with or without Intravenous Alteplase in Acute Stroke. N Engl J Med. May 21 2020;382(21):1981-1993. doi:10.1056/NEJMoa2001123
16. Suzuki K, Matsumaru Y, Takeuchi M, et al. Effect of Mechanical Thrombectomy Without vs With Intravenous Thrombolysis on Functional Outcome Among Patients With Acute Ischemic Stroke: The SKIP Randomized Clinical Trial. JAMA. Jan 19 2021;325(3):244-253. doi:10.1001/jama.2020.23522
17. Lodi Y, Reddy V, Petro G, Devasenapathy A, Hourani A, Chou CA. Primary acute stroke thrombectomy within 3 h for large artery occlusion (PAST3-LAO): a pilot study. J Neurointerv Surg. Apr 2017;9(4):352-356. doi:10.1136/neurintsurg-2015-012172
18. Perez de la Ossa N, Carrera D, Gorchs M, et al. Design and validation of a prehospital stroke scale to predict large arterial occlusion: the rapid arterial occlusion evaluation scale. Stroke. Jan 2014;45(1):87-91. doi:10.1161/STROKEAHA.113.003071
19. Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. Jan 1 2015;372(1):11-20. doi:10.1056/NEJMoa1411587
20. Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. Mar 12 2015;372(11):1009-18. doi:10.1056/NEJMoa1414792
21. Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. Mar 12 2015;372(11):1019-30. doi:10.1056/NEJMoa1414905
22. Molina CA, Chamorro A, Rovira A, et al. REVASCAT: a randomized trial of revascularization with SOLITAIRE FR device vs. best medical therapy in the treatment of acute stroke due to anterior circulation large vessel occlusion presenting within eight-hours of symptom onset. Int J Stroke. Jun 2015;10(4):619-26. doi:10.1111/ijs.12157
23. Powers WJ, Derdeyn CP, Biller J, et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 Guidelines for the Early Management of Patients With Acute Ischemic Stroke Regarding Endovascular Treatment: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. Oct 2015;46(10):3020-35. doi:10.1161/STR.0000000000000074
24. Albers GW, Marks MP, Kemp S, et al. Thrombectomy for Stroke at 6 to 16 Hours with Selection by Perfusion Imaging. N Engl J Med. Feb 22 2018;378(8):708-718. doi:10.1056/NEJMoa1713973
25. Nogueira RG, Jadhav AP, Haussen DC, et al. Thrombectomy 6 to 24 Hours after Stroke with a Mismatch between Deficit and Infarct. N Engl J Med.
26. Cagnazzo F, Derraz I, Dargazanli C, et al. Mechanical thrombectomy in patients with acute ischemic stroke and ASPECTS
27. Lima FO, Silva GS, Furie KL, et al. Field Assessment Stroke Triage for Emergency Destination: A Simple and Accurate Prehospital Scale to Detect Large Vessel Occlusion Strokes. Stroke. Aug 2016;47(8):1997-2002. doi:10.1161/STROKEAHA.116.013301
28. Birnbaum L, Wampler D, Shadman A, et al. Paramedic utilization of Vision, Aphasia, Neglect (VAN) stroke severity scale in the prehospital setting predicts emergent large vessel occlusion stroke. J Neurointerv Surg. Jun 2021;13(6):505-508. doi:10.1136/neurintsurg-2020- 016054
29. Chen S, Sun H, Lei Y, et al. Validation of the Los Angeles pre-hospital stroke screen (LAPSS) in a Chinese urban emergency medical service population. PLoS One. 2013;8(8):e70742. doi:10.1371/journal.pone.0070742